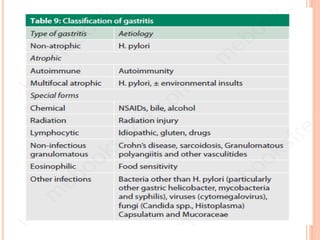
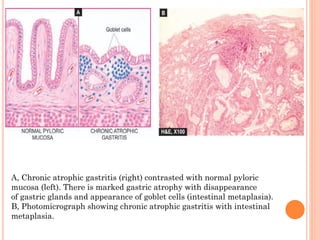
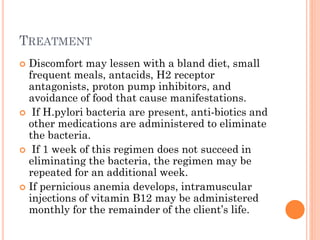
Chronic gastritis is long-term inflammation of the stomach lining that can be caused by H. pylori infection, autoimmune disorders, medications like NSAIDs, or stress. It is classified into types based on the affected stomach region and symptoms. Chronic gastritis may progress to gastric atrophy or intestinal metaplasia and increases the risk of peptic ulcers and gastric cancer. Treatment focuses on lifestyle changes like a bland diet and medication to reduce acid production.