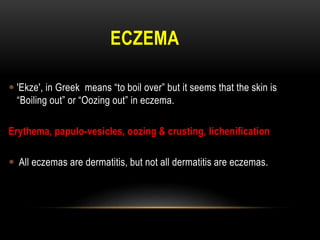
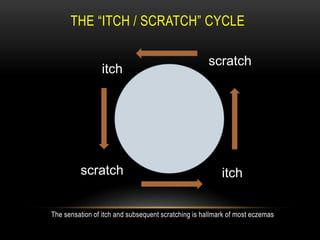
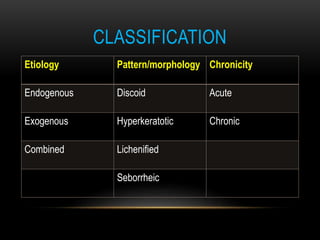
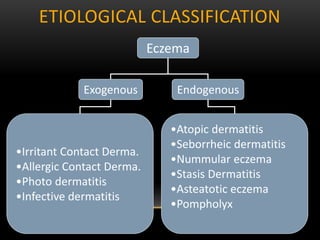
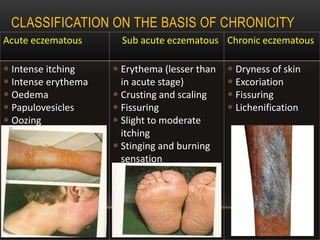
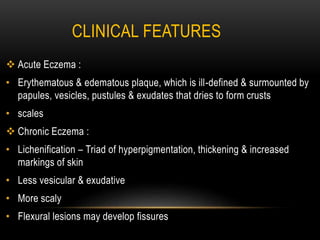
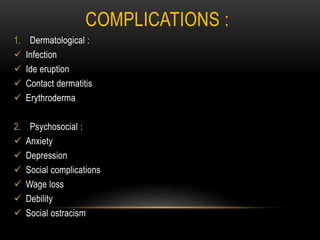
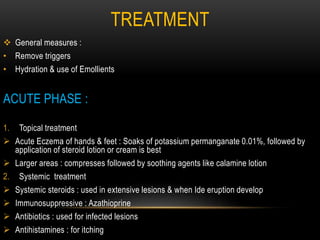
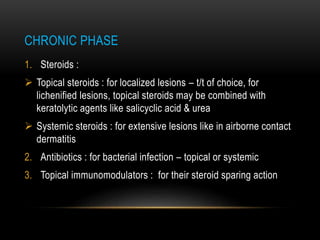
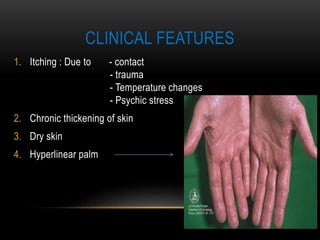
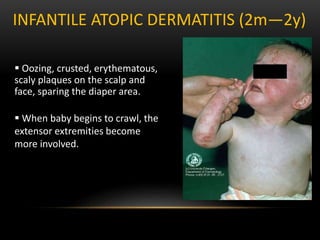
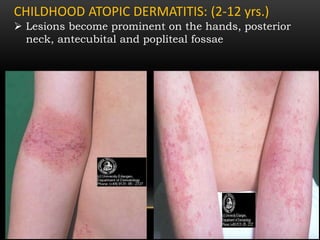
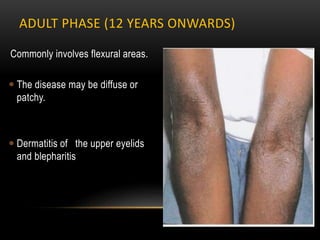
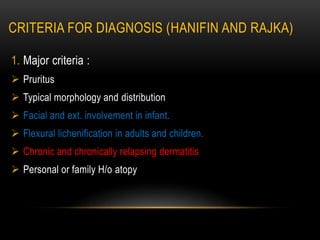
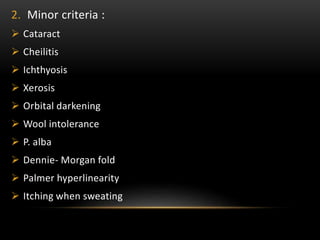
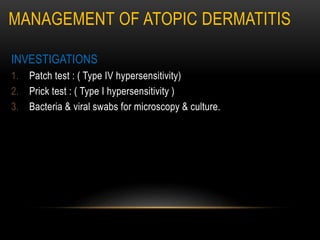
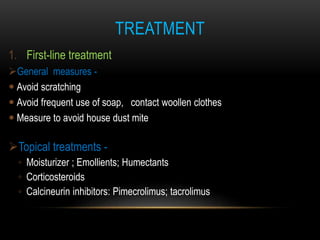
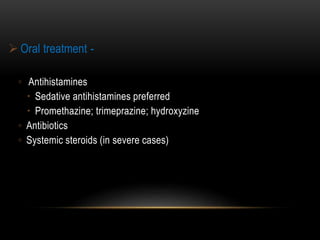
This document discusses eczema, including its classification, symptoms, and treatment. It begins by defining eczema as a skin condition characterized by itching and scratching. It then classifies eczema based on etiology, morphology, and chronicity. Symptoms of acute eczema include erythema, vesicles, and crusting, while chronic eczema features lichenification. Complications can be dermatological like infection or psychosocial like anxiety. Treatment involves identifying triggers, moisturizing, and using topical corticosteroids or immunosuppressants. It also focuses on atopic dermatitis, its causes, features in infants/children/adults, and management through avoidance of