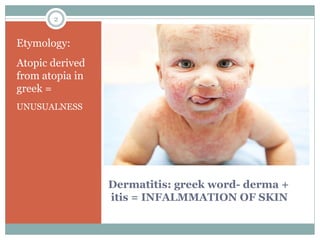
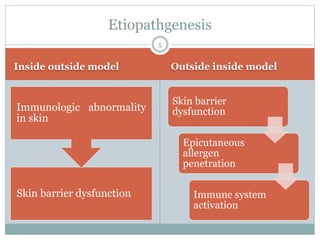
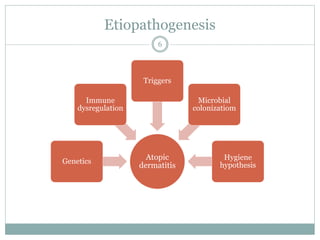
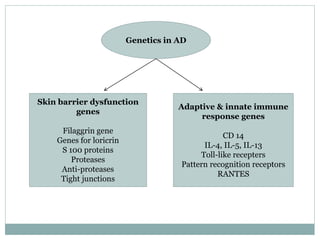
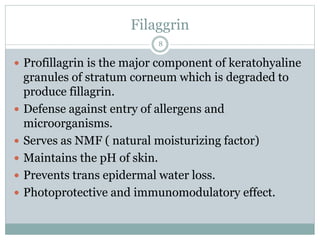
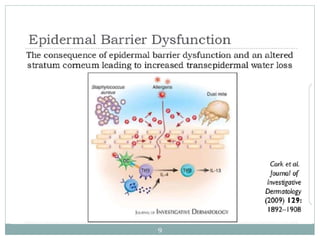
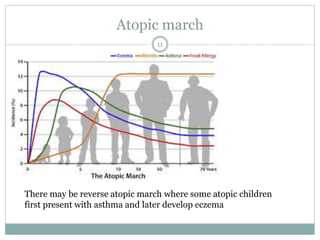
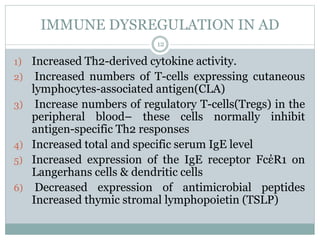
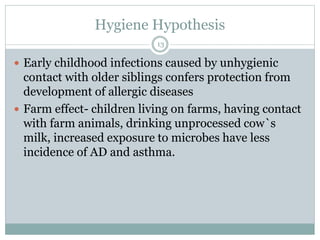
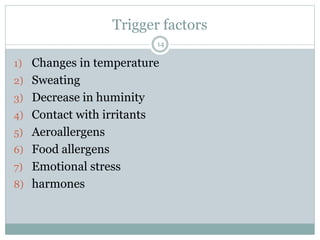
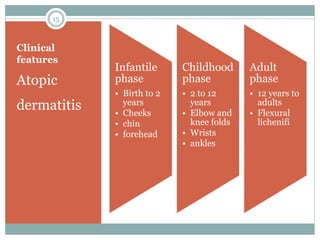
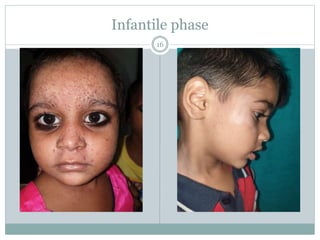
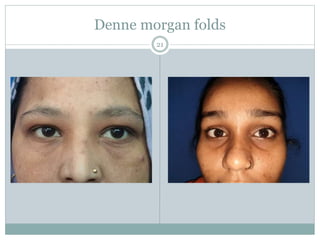
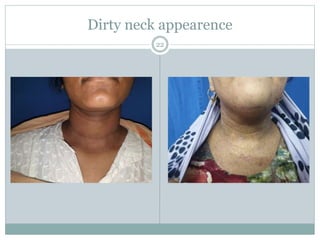
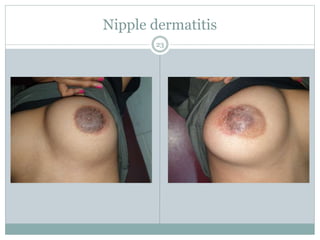
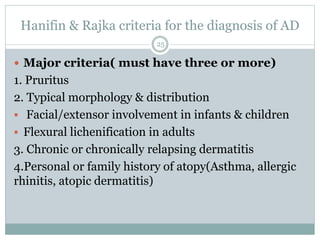
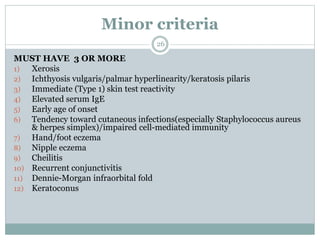
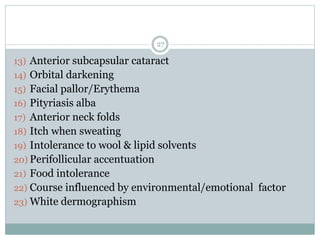
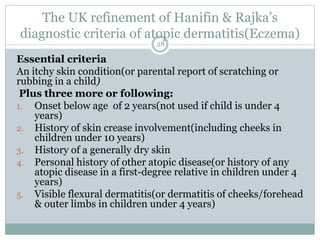
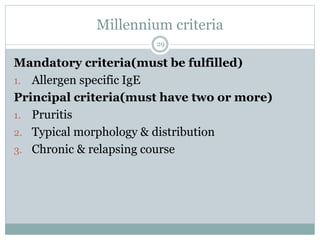
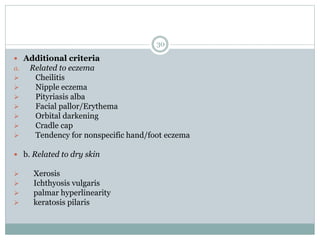
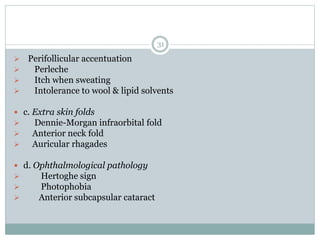
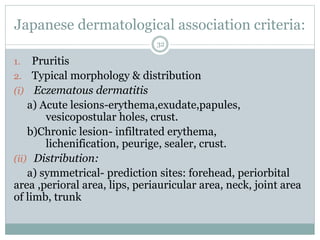
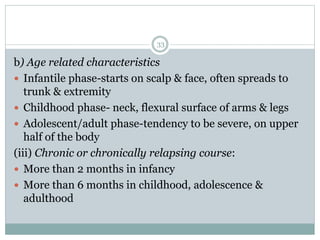
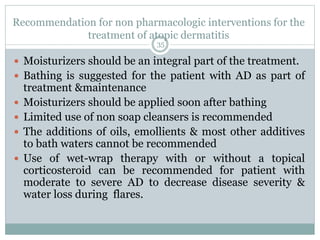
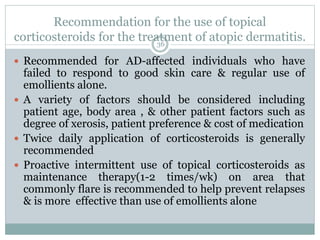
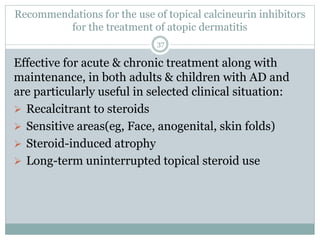
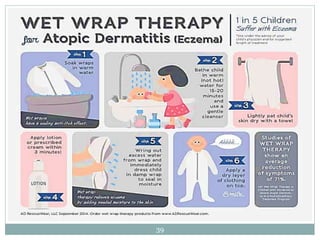
The document provides a comprehensive overview of atopic dermatitis, detailing its etiology, clinical features, and genetic components, along with diagnostic criteria and management guidelines. It emphasizes the role of immune dysregulation, triggers, and the importance of moisturization and topical treatments in managing the condition. The document also discusses the concept of the atopic march and highlights various treatment modalities, including non-pharmacologic interventions and pharmacological therapies.