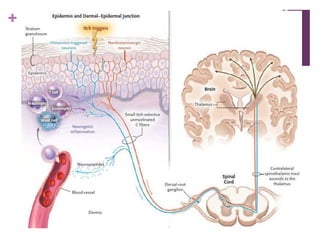
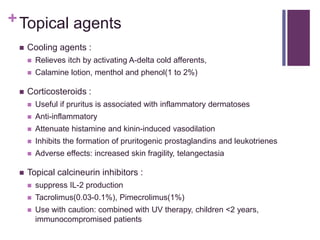
Pruritus, or itch, is a sensation that provokes the desire to scratch. Chronic pruritus lasts more than 6 weeks and can be caused by skin diseases or systemic diseases. Itch is transmitted through unmyelinated C fibers and is a distinct sensation from pain. Scratching provides temporary relief by stimulating myelinated fibers or damaging sensory nerve endings. Management of pruritus involves general skin care, topical agents like corticosteroids, calcineurin inhibitors, local anesthetics, and antihistamines, as well as treating any underlying cause.