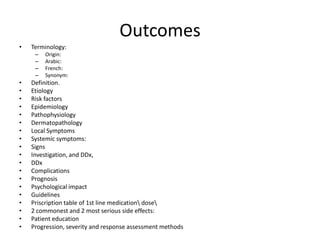
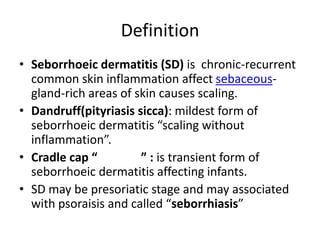
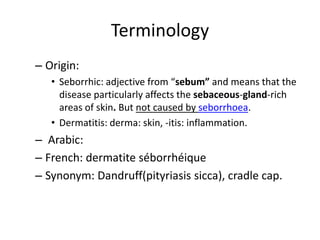
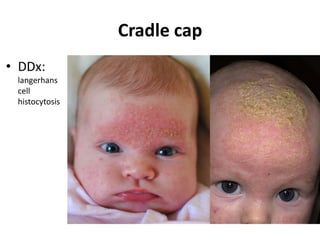
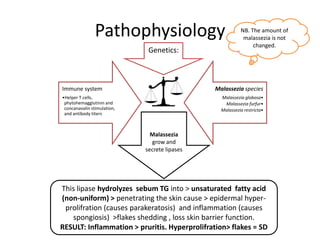
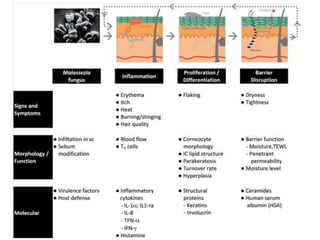
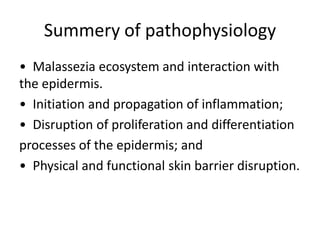
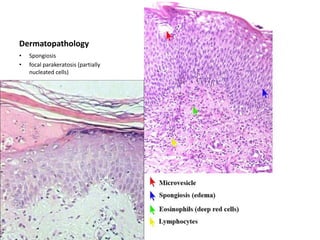
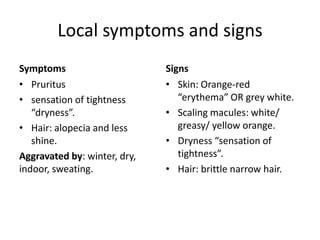
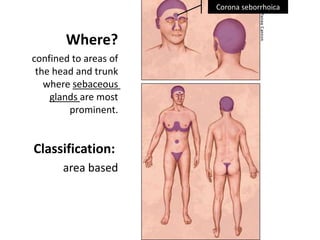
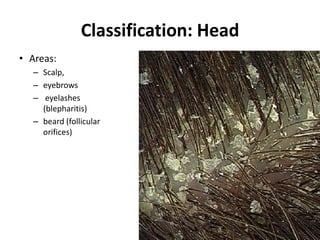
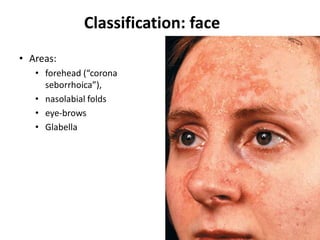
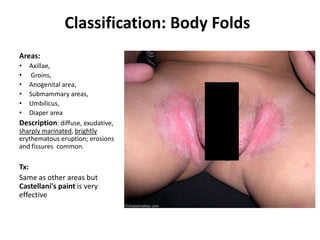
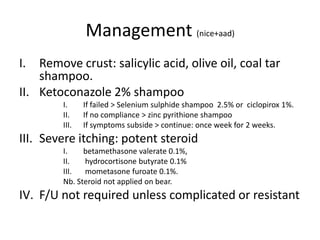
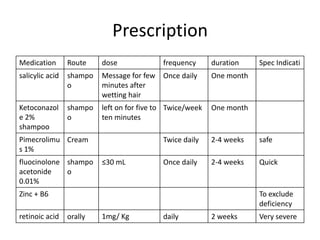
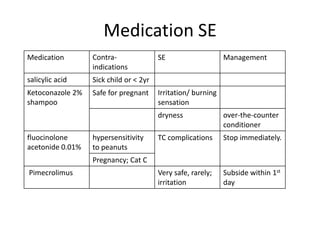
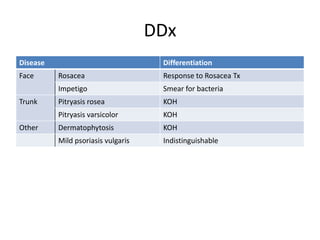
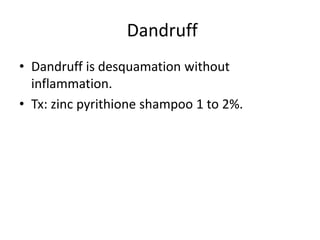
The document provides a comprehensive overview of seborrheic dermatitis, detailing its definition, etiology, risk factors, epidemiology, pathophysiology, and management guidelines. It highlights the condition's clinical symptoms and signs, especially its effects on sebaceous-gland-rich areas of the skin, while offering insight into common treatments and their complications. The document also includes differential diagnoses and emphasizes the importance of patient education and follow-up care.