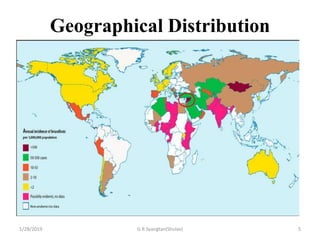
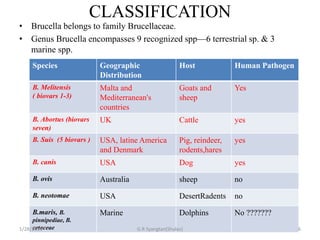
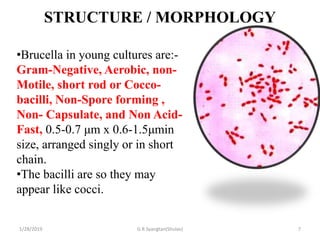
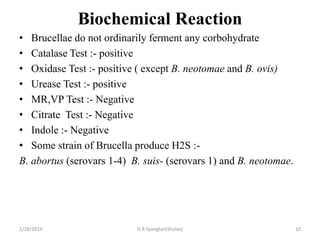
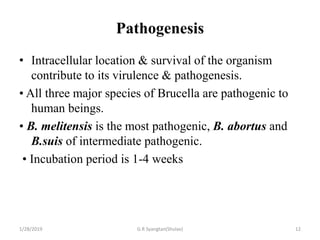
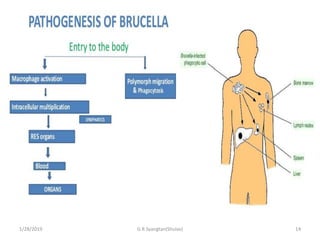
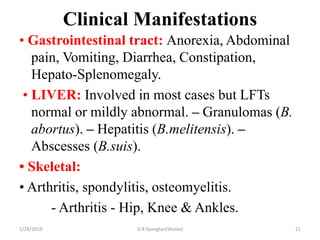
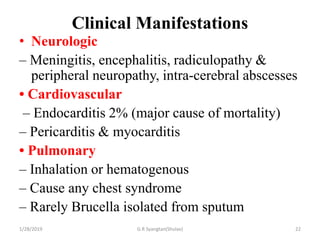
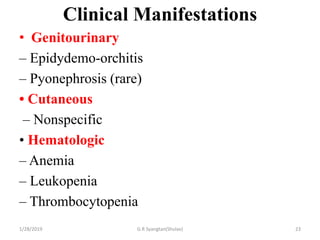
Brucellosis is a zoonotic infection caused by the Brucella species, primarily affecting domesticated animals and transmitted to humans through contaminated animal products. Symptoms of brucellosis can range from mild to severe and include fever, fatigue, and joint pain, while diagnosis often involves blood cultures and serological tests. Treatment typically includes antibiotics, and prevention relies on controlling the disease in animal populations and avoiding unpasteurized products.