This document describes three examples of case-control study designs:
1) A nested case-control study examining the association between antipsychotic drugs and venous thromboembolism using a large UK database.
2) A cumulative case-control study investigating a diarrhea outbreak in India to identify risk factors.
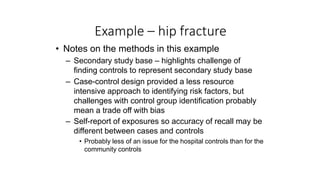
3) A case-control study comparing hospital and community controls to identify risk factors for hip fracture.