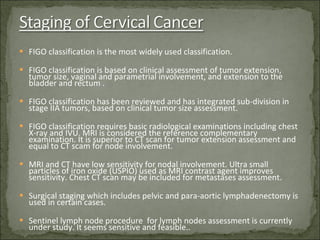
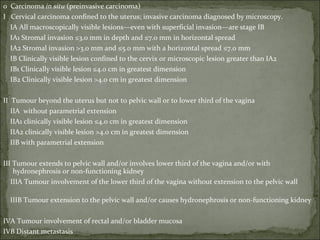
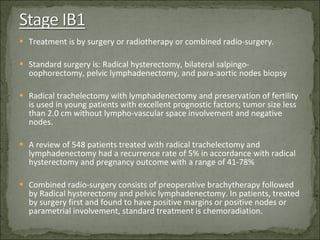
Nearly 500,000 new cases of cervical cancer occur worldwide each year, with the majority in developing countries. Infection with HPV is responsible for virtually all cervical cancer cases. Screening includes Pap smears and HPV testing, while vaccination may prevent up to 70% of cases but is not widely available due to cost. Diagnosis is through biopsy and histopathological examination, while staging uses the FIGO system based on tumor size and spread. Treatment depends on stage but commonly includes surgery such as hysterectomy with or without radiation or chemotherapy.