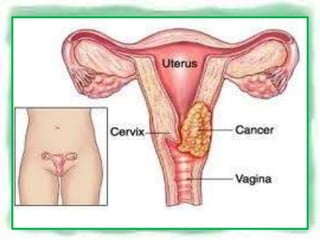
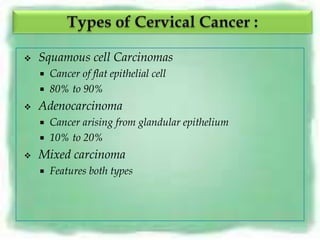
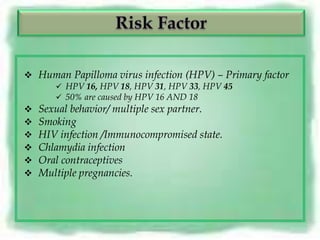
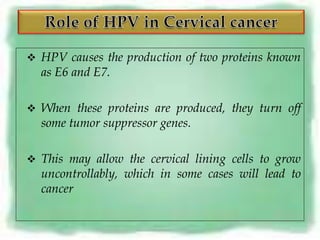
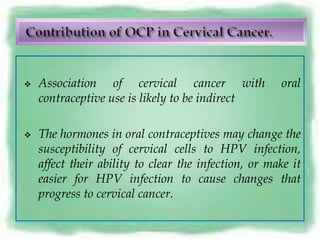
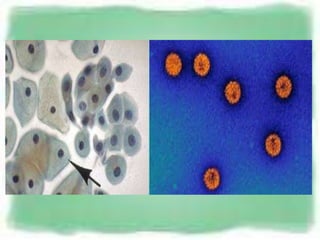
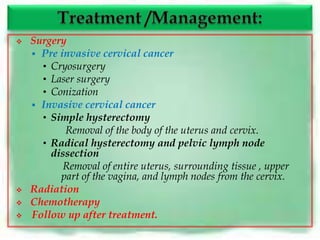
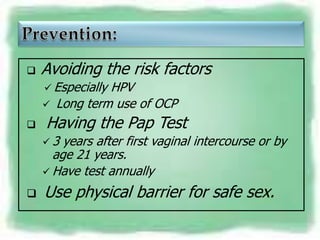
The document discusses cervical cancer, including that it occurs in the cervix and is caused by HPV infection. It notes that over 2000 new cases are detected in Nepal each year. The main types are squamous cell carcinoma and adenocarcinoma. Risk factors include HPV, multiple sex partners, smoking, and HIV/AIDS. Symptoms can include abnormal bleeding. Screening includes Pap tests and colposcopy with biopsies for diagnosis. Treatment options are surgery, radiation, and chemotherapy, with follow up after treatment. Prevention includes avoiding risk factors and regular Pap screening.