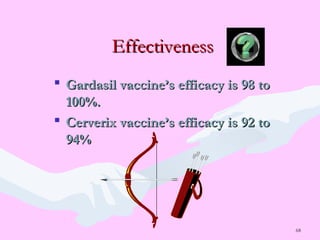
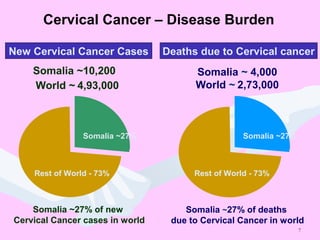
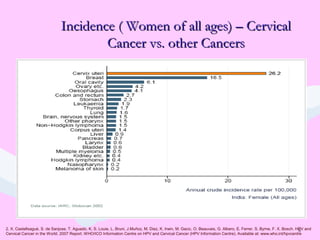
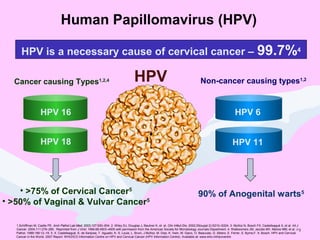
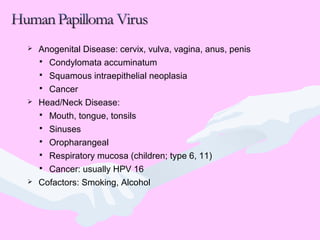
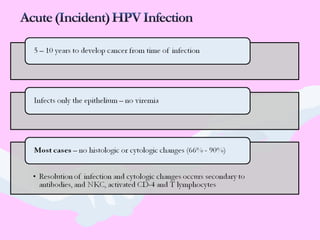
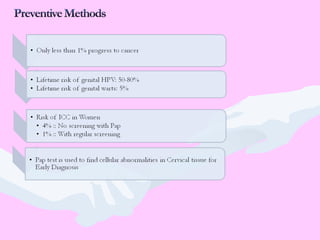
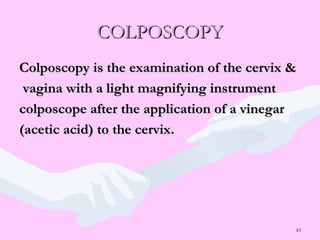
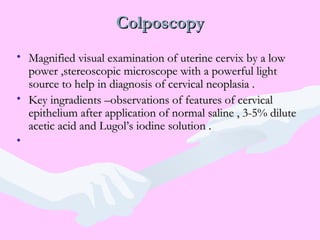
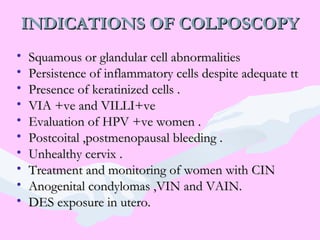
Cervical cancer significantly impacts women in Somalia, with 50 deaths daily due to the disease. The document discusses the importance of prevention through HPV vaccination, screening, and early detection methods such as Pap smears and colposcopy. Emphasizing that cervical cancer is largely preventable, it highlights various risk factors, symptoms, and the necessity for regular health checks.





![How to take a Pap Smear ?
Spatula is rotated through 360 degrees
maintaining contact with ectocervix
Do not use too much force [bleeding /pain]
Do not use too less force [inadequate sample]
Sample is smeared evenly on the slide and fixed
immediately
Both sides of spatula are to be smeared](https://image.slidesharecdn.com/cervicalcancertalk-161111054959/85/CERVICAL-CANCER-ITS-PREVENTION-35-320.jpg)
![How to take a Pap Smear ?
Endocervical sample is collected using an
endocervical brush
Insert the cytobrush into canal, so that last bristles
of brush are visible
Rotate the brush through 180 degrees. [more
rotations increase the chance of bleeding]
Sample is rolled on the slide and fixed.](https://image.slidesharecdn.com/cervicalcancertalk-161111054959/85/CERVICAL-CANCER-ITS-PREVENTION-36-320.jpg)








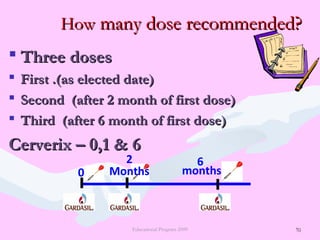
![65
Primary PreventionPrimary Prevention
by HPV Vaccineby HPV Vaccine
GARDASILGARDASIL®®
[Human Papillomavirus Quadrivalent[Human Papillomavirus Quadrivalent
(Types 6, 11, 16, and 18)(Types 6, 11, 16, and 18)
Vaccine 0.5ml prefilled syringe]Vaccine 0.5ml prefilled syringe]
CERVERIXCERVERIX
[Human Papillomavirus Bivalent[Human Papillomavirus Bivalent
(Types 16 and 18)(Types 16 and 18)
Vaccine 0.5ml prefilled syringe]Vaccine 0.5ml prefilled syringe]
09-2009-GRD-2008-AP-(IN)-1601-SS](https://image.slidesharecdn.com/cervicalcancertalk-161111054959/85/CERVICAL-CANCER-ITS-PREVENTION-65-320.jpg)