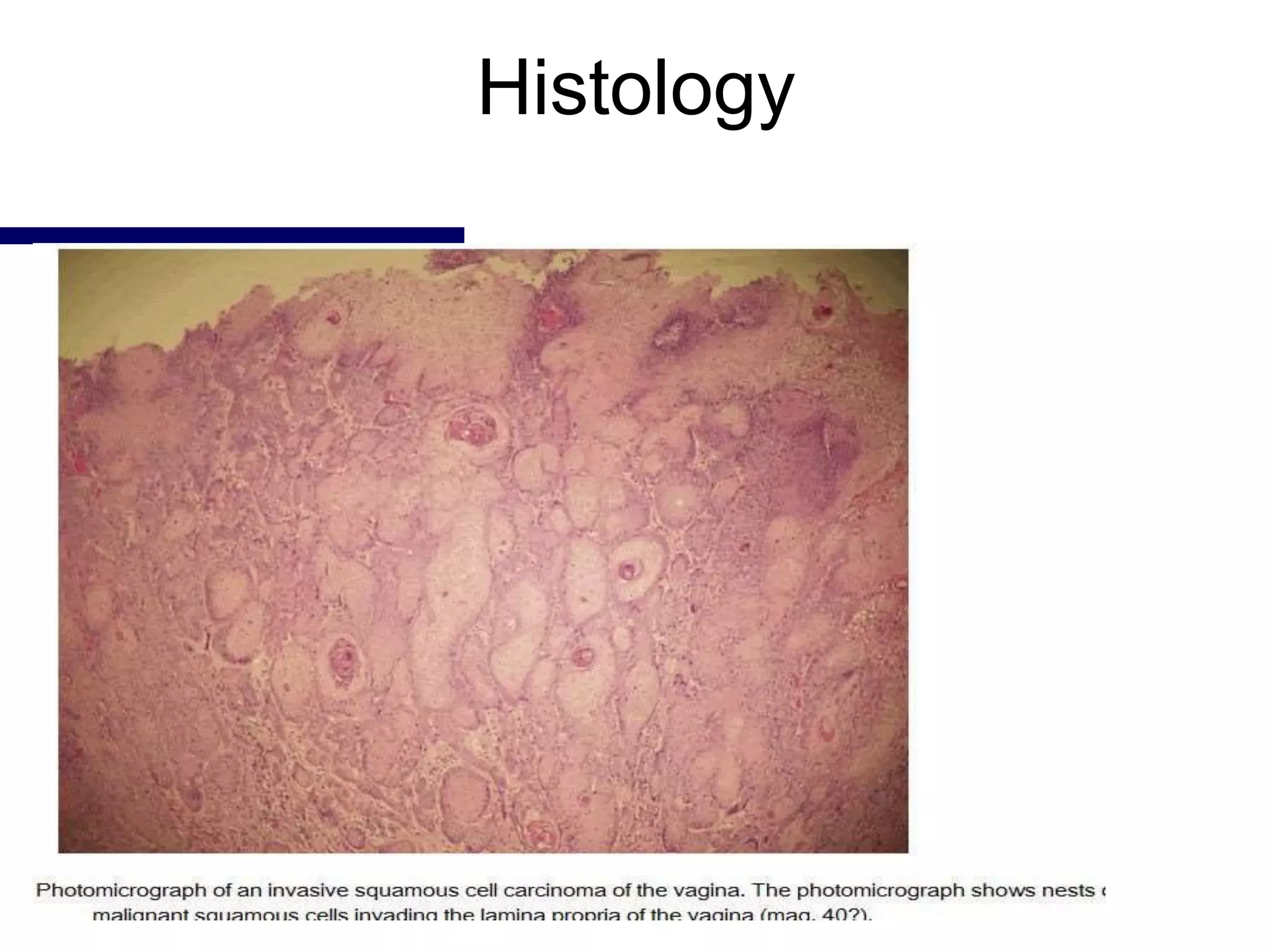
1. Carcinoma of the vagina is a rare cancer representing 1-2% of gynecologic malignancies. The majority are squamous cell carcinomas.
2. Risk factors include HPV infection, previous pelvic radiation, and in-utero exposure to DES which can cause clear cell adenocarcinoma.
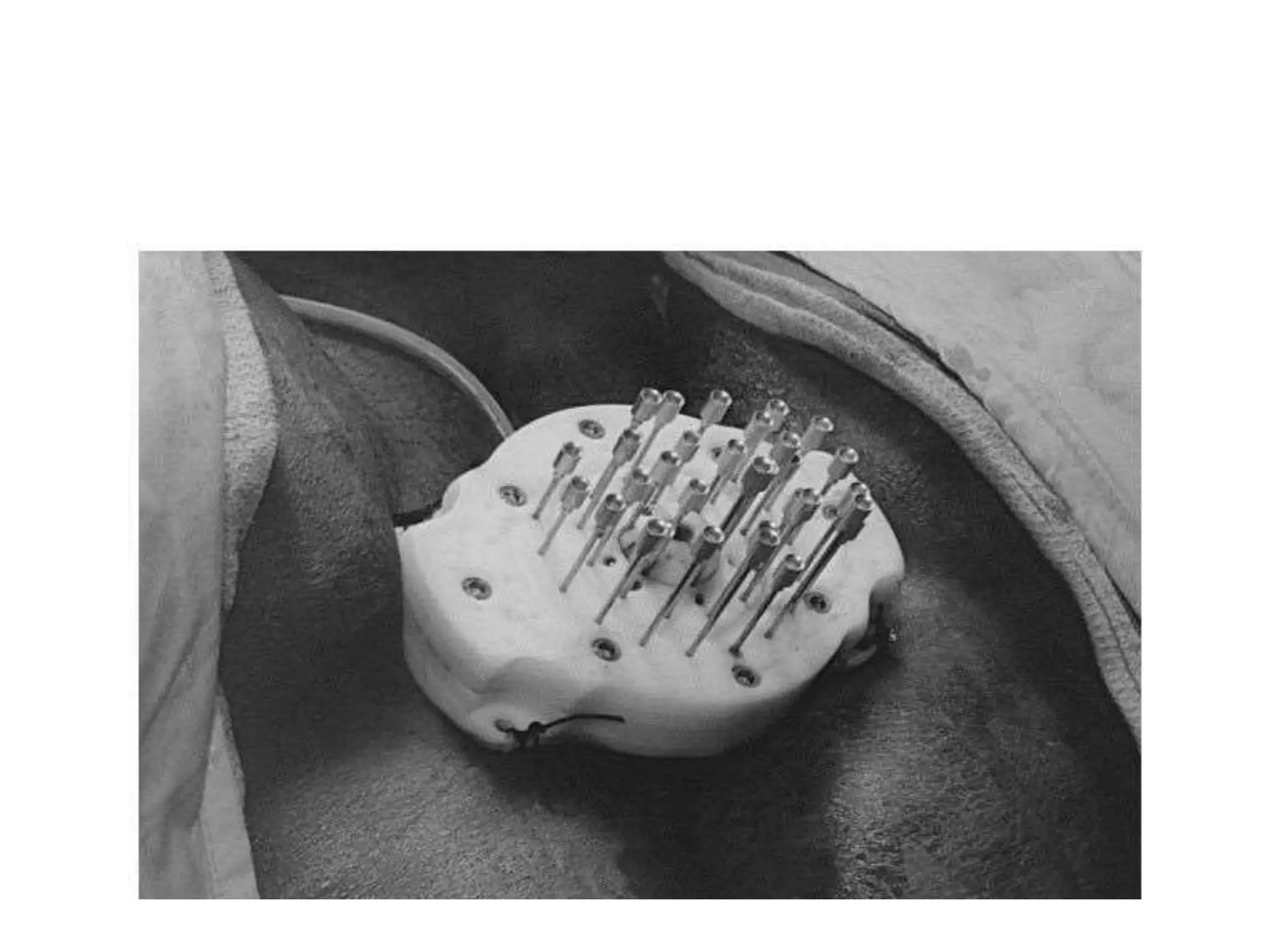
3. Treatment depends on stage but commonly involves radiation therapy with brachytherapy. Surgery may be used for early stage lesions or failures of radiation therapy. Chemotherapy combined with radiation may improve outcomes for advanced stages.