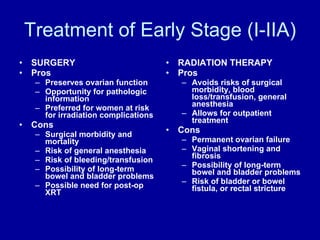
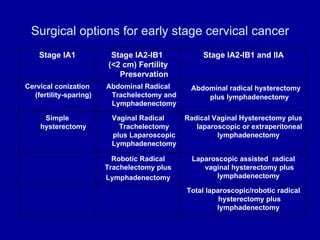
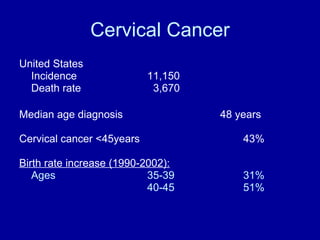
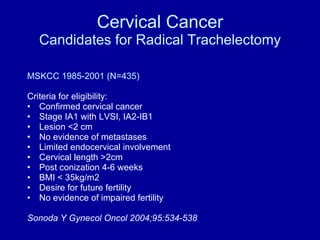
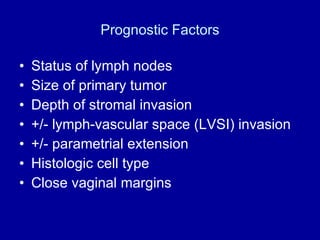
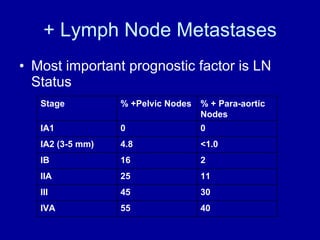
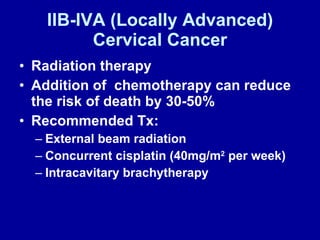
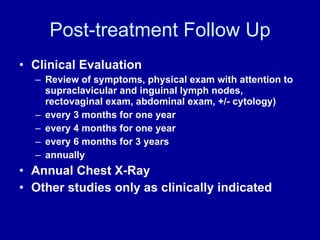
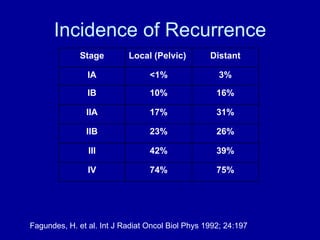
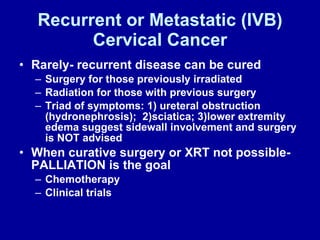
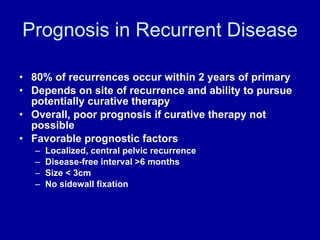
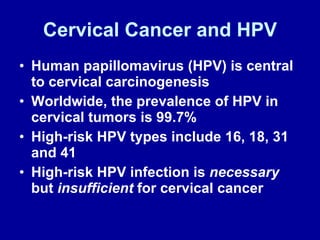
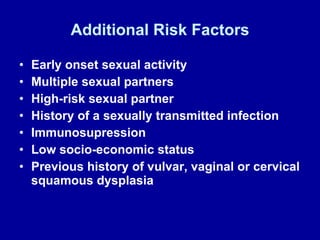
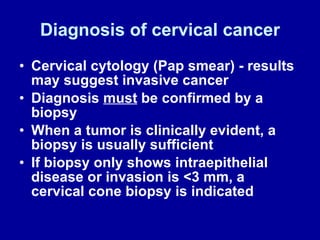
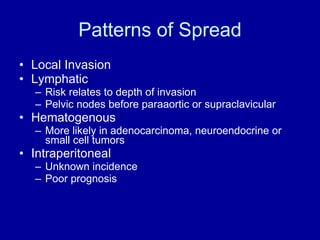
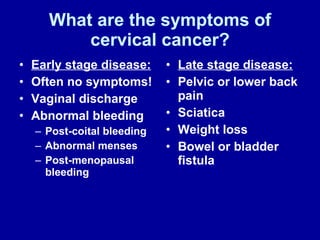
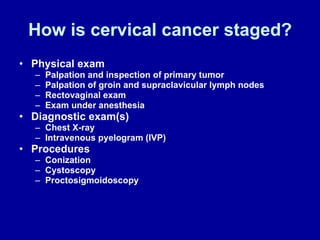
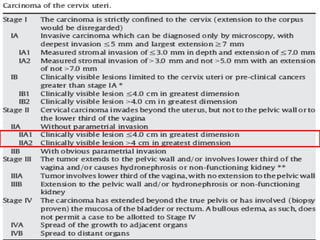
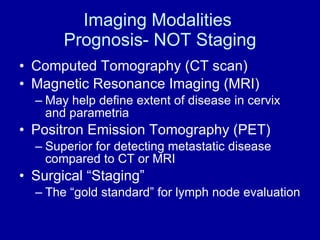
Cervical cancer is the second-leading cause of cancer mortality in women globally, with a significant prevalence of human papillomavirus (HPV) in cervical tumors. Early detection through cervical cytology and various treatment options, including surgery and chemoradiation, are crucial, particularly in low-resource settings. The prognosis depends on the stage of cancer, with comprehensive follow-ups and possible palliative care for recurrent cases.
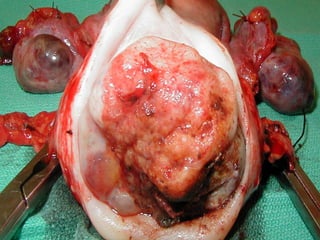
![Stage Determines Treatment Early Stage (I-IB1 [IB2-IIa]) Primary Surgery Chemoradiation Locally Advanced(IB2-IVA) Primary Chemoradiation Disease with Distant Metastases (IVB) Systemic chemotherapy](https://image.slidesharecdn.com/cervicalcancer-guatemala1-101206155821-phpapp01/85/Cervical-Cancer-15-320.jpg)