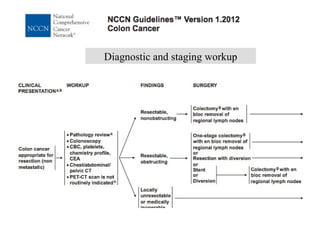
The document discusses guidelines for screening, diagnosis, staging, adjuvant therapy, advanced disease treatment, and follow-up for colorectal cancer from both the ESMO and NCCN perspectives. It provides recommendations for screening the general and high-risk populations. It also outlines the diagnostic and staging workup, including endoscopy, biopsy, imaging, and surgical staging. Guidelines are presented for adjuvant therapy based on cancer stage. Recommendations are provided for managing both synchronous and metachronous metastatic disease, as well as rectal cancer treatment.