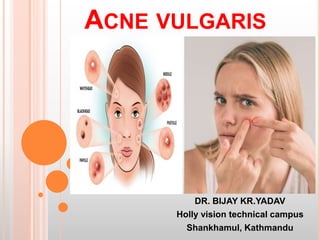
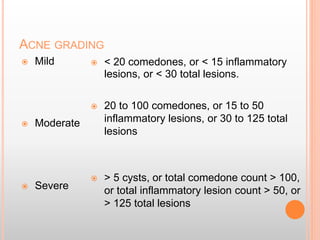
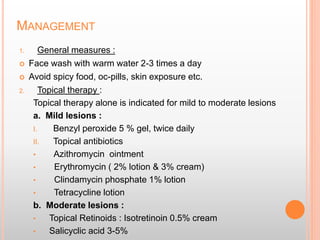
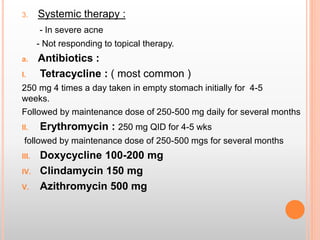
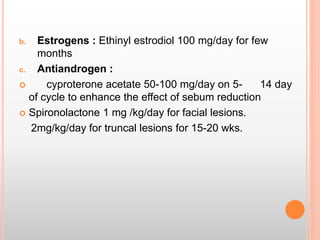
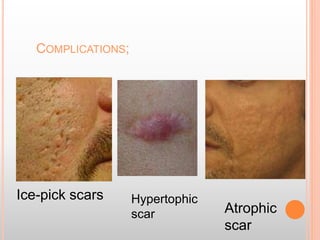
Acne vulgaris is the most common skin condition affecting teenagers, characterized by inflammatory and non-inflammatory lesions on the face, neck and upper trunk. It peaks in late teens and usually stops by age 25. Factors like hormones, stress, and certain foods can aggravate acne. Treatment involves topical medications for mild to moderate acne and oral antibiotics or hormones for more severe cases. Complications may include scarring. Proper long-term treatment and management is important to prevent recurrence and worsening of acne over time.