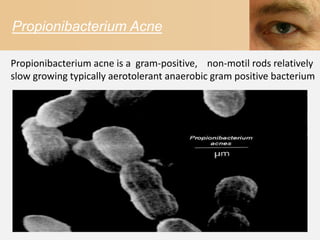
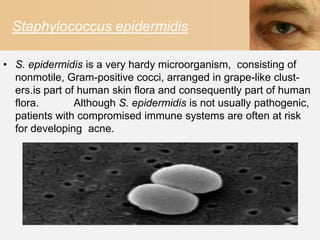
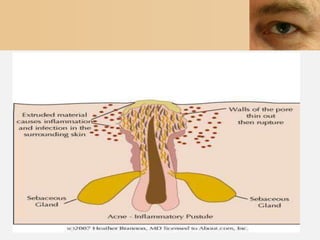
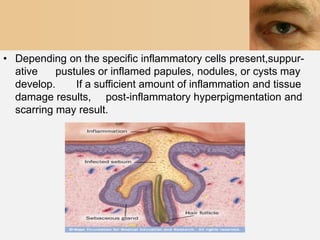
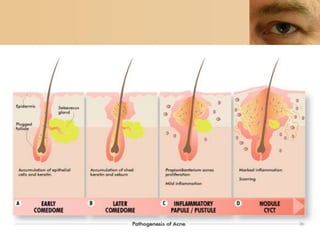
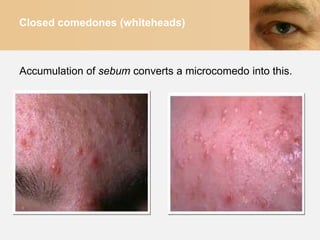
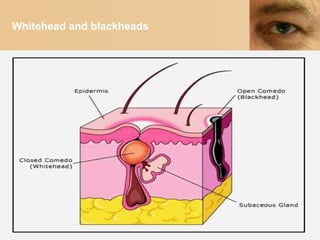
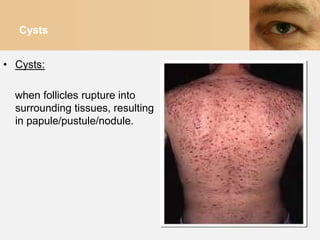
Acne vulgaris, or common acne, is a chronic inflammatory skin condition characterized by abnormalities in sebum production, follicular desquamation, bacterial proliferation and inflammation. It is the most common skin disorder, affecting over 17 million Americans. The main causes are P. acnes and S. epidermidis bacteria colonizing hair follicles and stimulating inflammation. Clinical manifestations range from non-inflammatory whiteheads and blackheads to inflammatory papules, pustules, cysts and nodules. Treatment focuses on reducing inflammation and preventing complications using topical and oral medications like benzoyl peroxide, antibiotics and retinoids. While acne usually resolves by the mid-20s, some patients