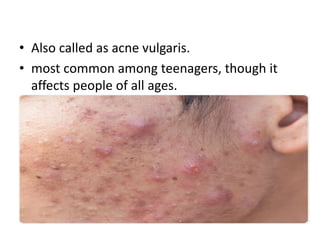
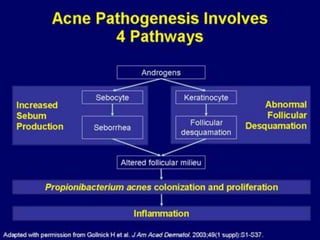
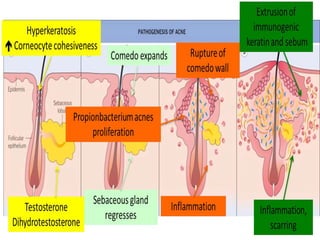
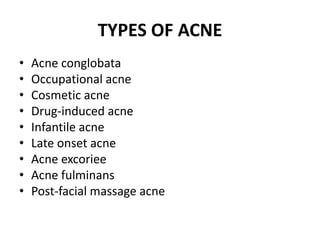
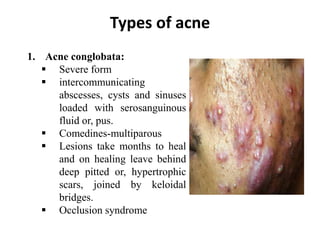
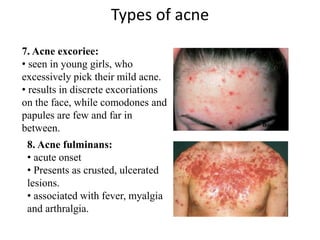
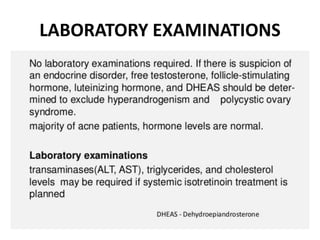
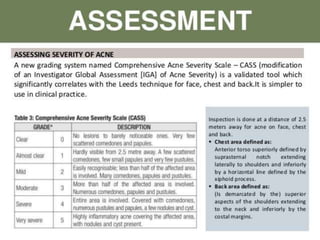
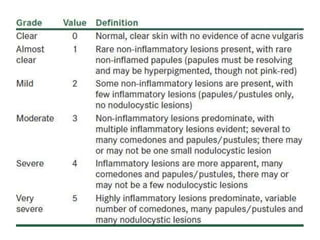
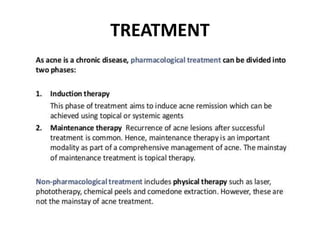
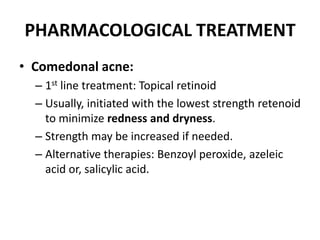
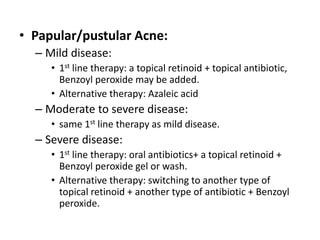
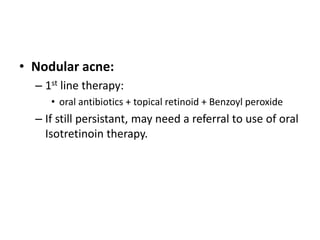
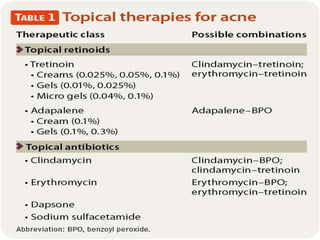
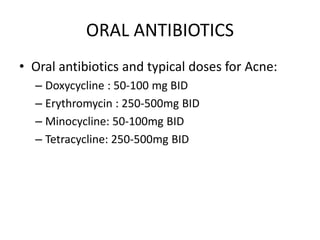
Acne is a common skin condition caused by clogged hair follicles and bacterial infection. It presents as whiteheads, blackheads, pimples, and deeper lumps. Risk factors include genetics and hormones. Types include infantile acne, drug-induced acne, and acne fulminans. Treatment involves topical retinoids and antibiotics for mild to moderate acne, with oral antibiotics and isotretinoin for more severe cases.