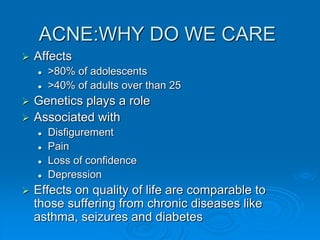
This document provides an overview of acne, including its causes, clinical presentation, differential diagnosis, and treatment options. It discusses the pathophysiology of acne and how hormones can contribute to its development during puberty. A variety of treatment approaches are described for mild, moderate, and severe acne, including topical retinoids, antibiotics, benzoyl peroxide, oral contraceptives, antibiotics, and isotretinoin for more severe cases. The document also reviews potential side effects of different acne medications.