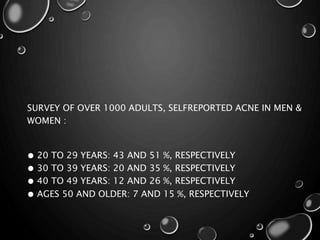
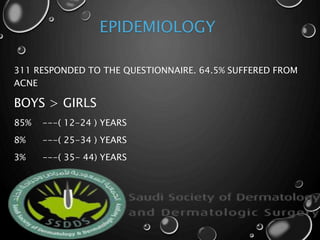
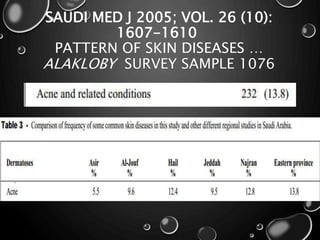
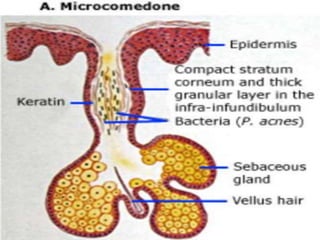
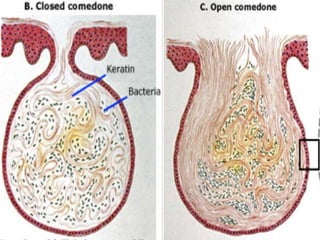
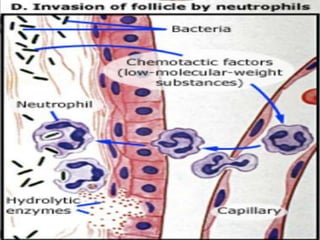
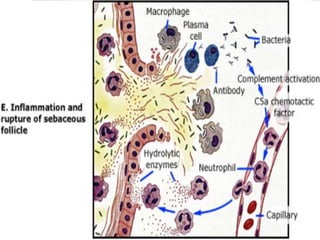
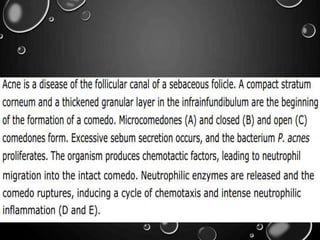
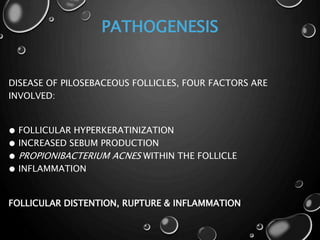
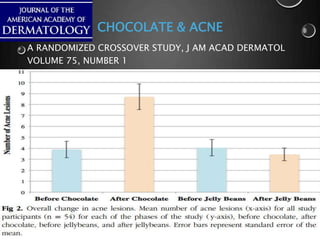
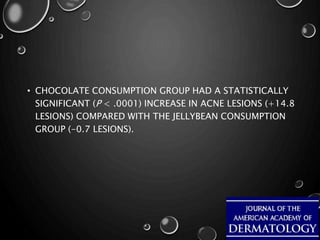
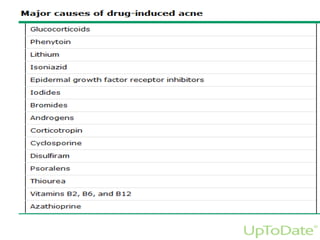
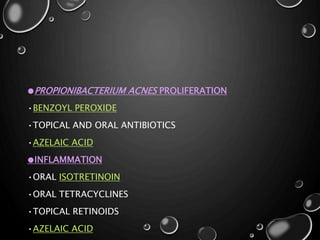
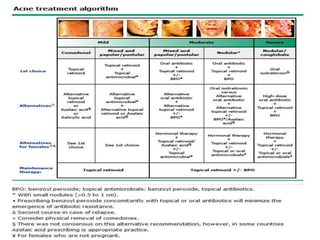
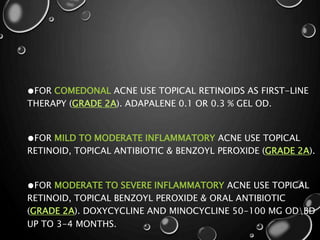
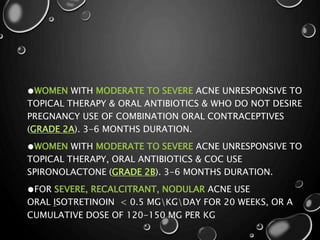
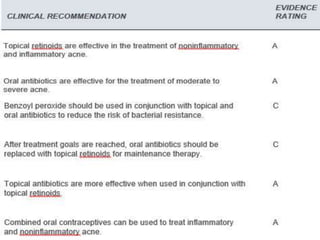
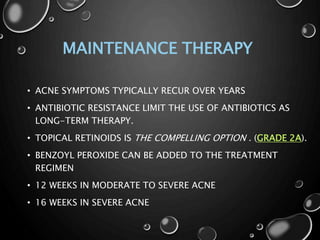
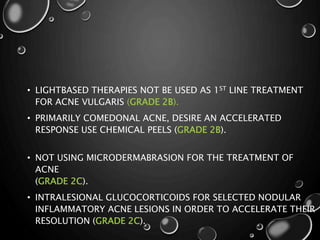
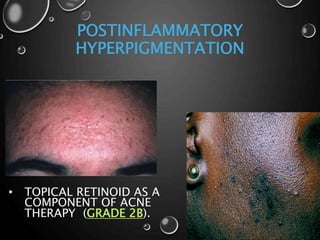
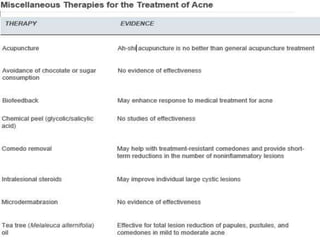
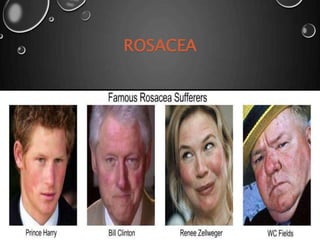
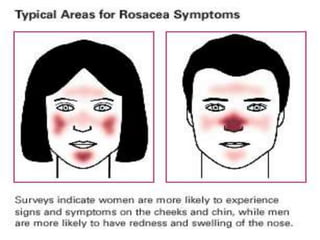
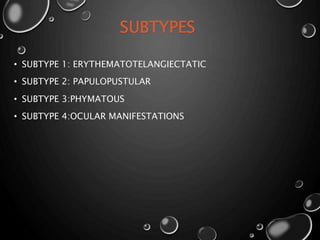
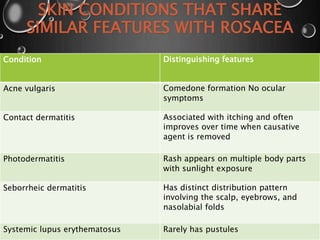
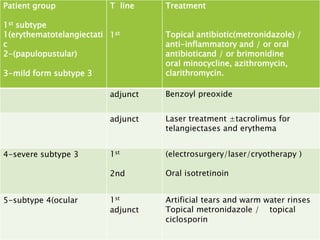
This document discusses the management of acne and rosacea. It defines the diseases, their clinical manifestations and risk factors. For acne, treatment involves targeting the four pathological factors with topical retinoids, antibiotics, isotretinoin or hormonal therapies depending on severity. Maintenance therapy typically involves topical retinoids. Rosacea management focuses on subtypes and includes lifestyle changes, topical metronidazole and oral antibiotics. Both conditions require long-term management to control symptoms and prevent scarring. Referral is indicated for severe or refractory cases.