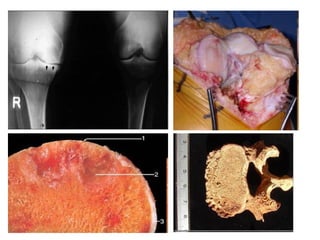
This document discusses bone structure and diseases. It describes the cells that make up and remodel bone, including osteoprogenitors, osteoblasts, osteoclasts, and osteocytes. It also discusses the proteins and minerals that compose bone tissue. A variety of bone diseases are outlined including malformations, diseases of bone cells and proteins, metabolic diseases, diseases of decreased or abnormal bone mass, tumors, fractures, osteonecrosis, osteomyelitis, and other conditions. Specific bone tumors are also described such as osteochondroma, chondroma, chondroblastoma, and osteosarcoma.































![FRACTURES
• THREE PHASES
– HEMATOMA, minutes days PGDF, TGF-β,
FGF
– SOFT CALLUS (“PRO”-CALLUS), ~1 week
– HARD CALLUS (BONY CALLUS), several
weeks
• COMPLICATIONS
– PSEUDARTHROSIS
– INFECTION (especially OPEN [communicating]
fractures)](https://image.slidesharecdn.com/27-ortho-140902155754-phpapp01/85/27-ortho-33-320.jpg)















































![JOINT DISEASES
•“ARTHRITIS”
– DEGENERATIVE (OSTEOARTHRITIS)
– RHEUMATOID
– “JUVENILE” RHEUMATOID
– NON-INFECTIOUS: Ankylosing Spond.,
Reactive, Psoriasis, IBD
– INFECTIOUS: Supp., TB, Lyme, Viral
– GOUT (URATE)
– PSEUDOGOUT (PYROPHOSPHATE)
• Tumors
– Ganglion (Synovial Cyst)
– Giant Cell Tumor (Pigmented VilloNodular Synovitis[PVNS])
– Synovial Sarcoma](https://image.slidesharecdn.com/27-ortho-140902155754-phpapp01/85/27-ortho-84-320.jpg)









![“SERONEGATIVE” ARTHRITIDES
• ANKYLOSING SPONDYLITIS (aka,
“rheumatoid” spondylitis, or Marie-
Strumpell Disease [HLA-B27] (M>>F)
• “REACTIVE” ARTHRITIS (FOLLOWS
GU or GI INFECTIONS)
–REITER SYDROME (urethral &
conjunctival inflammation too) [HLA-B27]
–Arthritis associated with IBD
• PSORIATIC ARTHRITIS](https://image.slidesharecdn.com/27-ortho-140902155754-phpapp01/85/27-ortho-95-320.jpg)