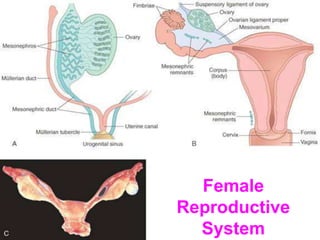
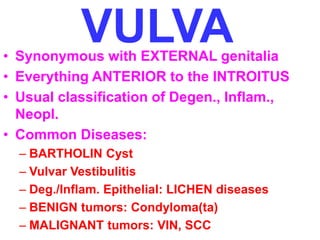
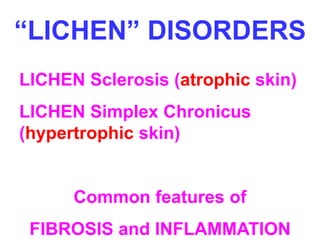
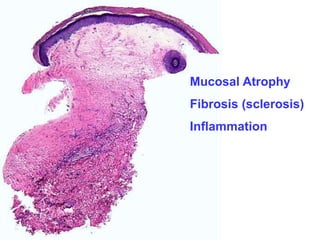
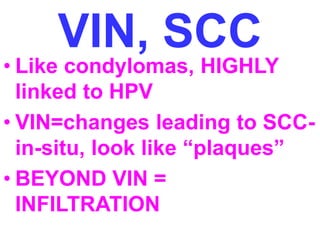
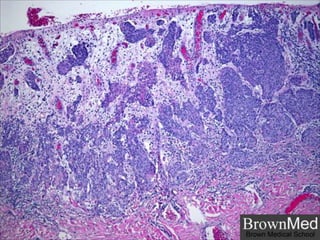
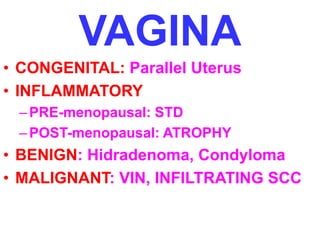
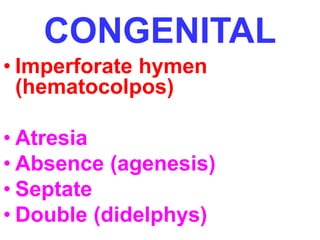
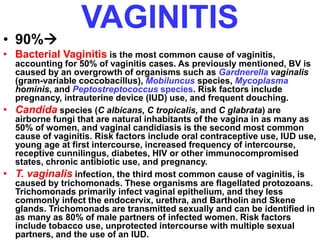
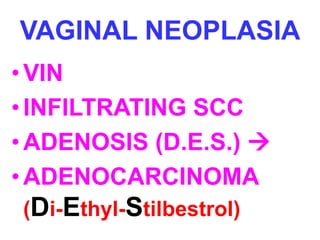
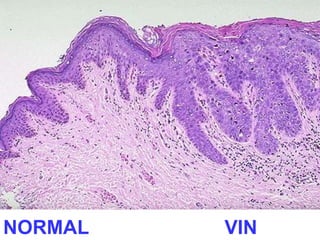
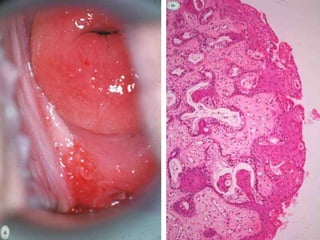
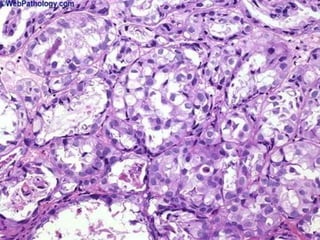
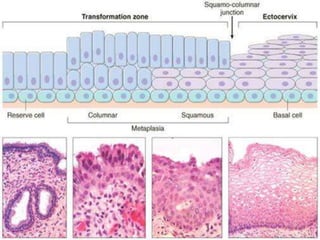
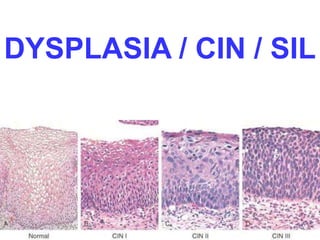
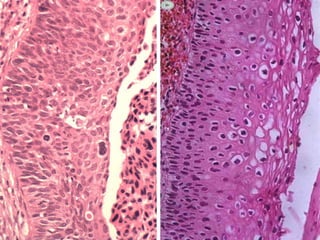
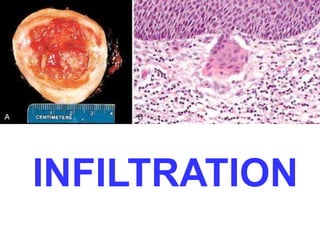
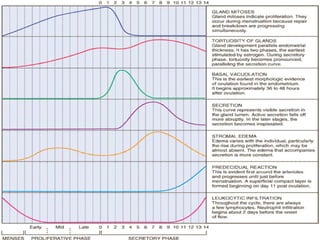
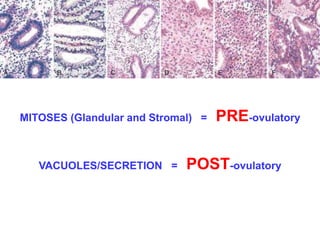
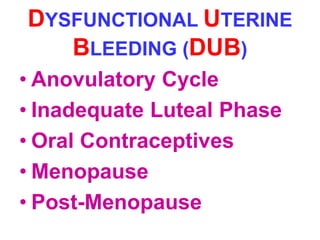
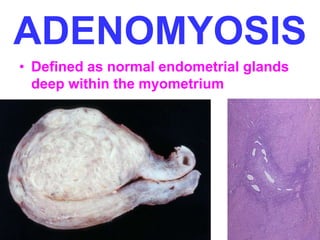
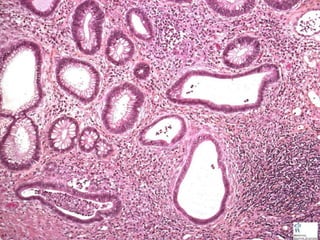
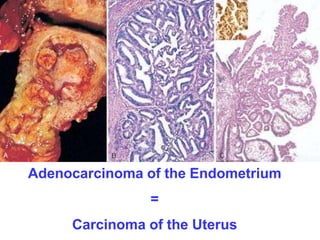
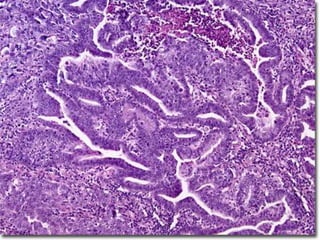
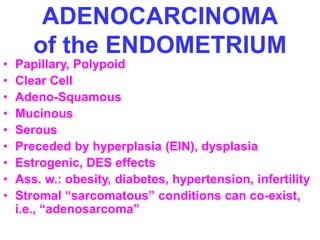
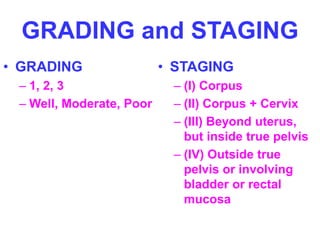
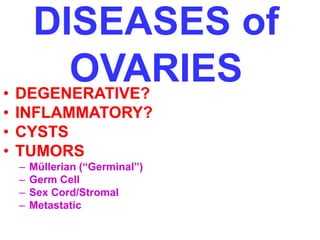
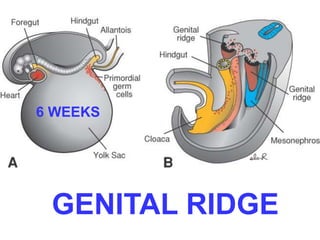
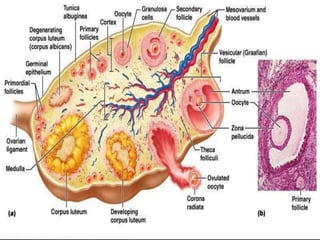
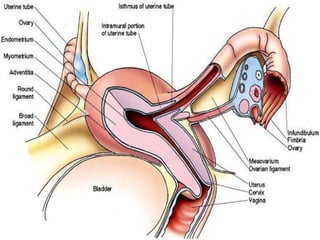
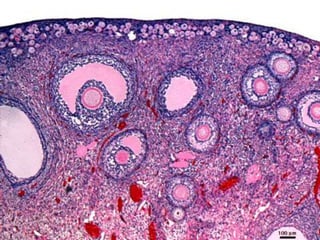
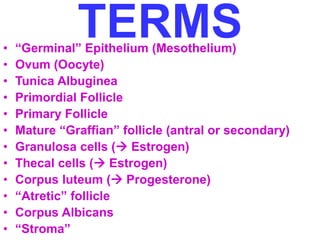
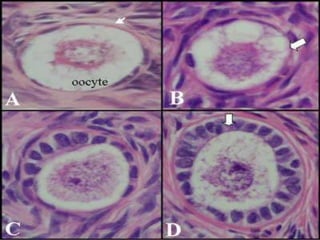
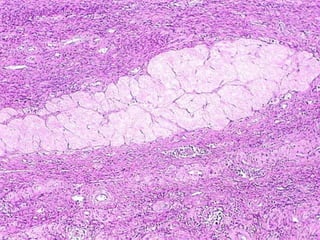
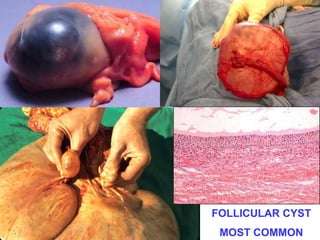
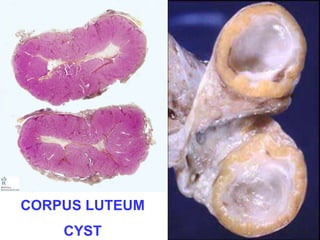
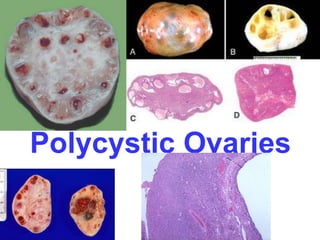
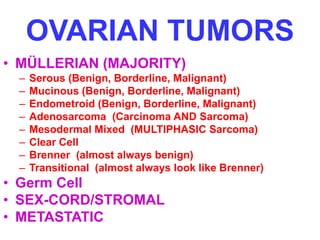
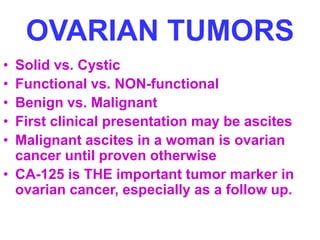
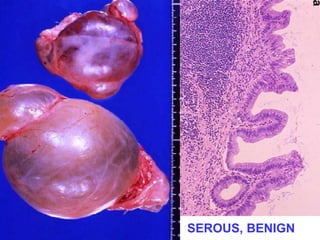
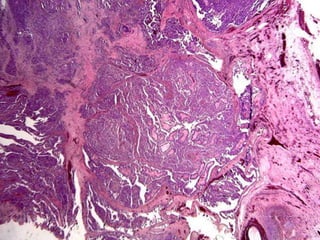
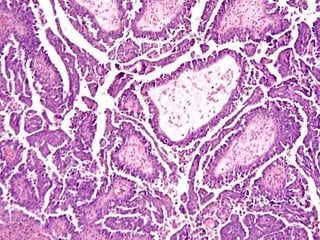
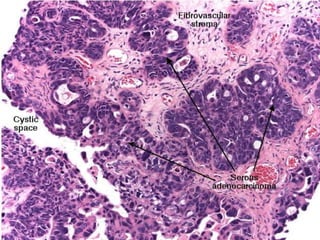
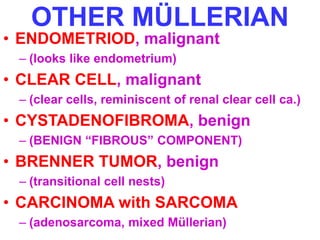
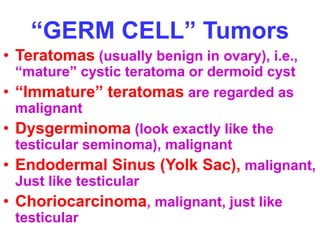
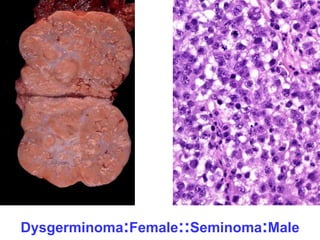
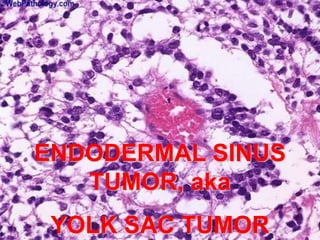
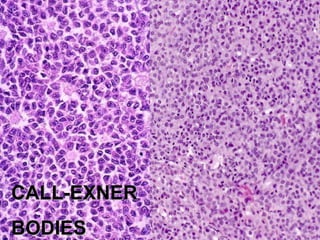
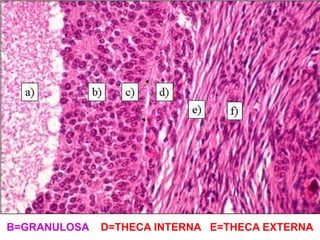
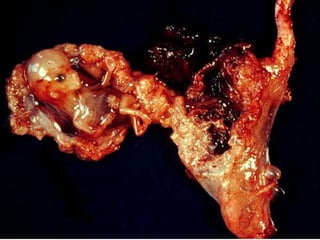
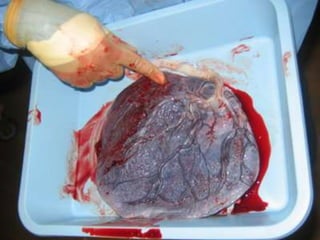
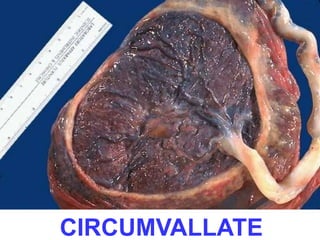
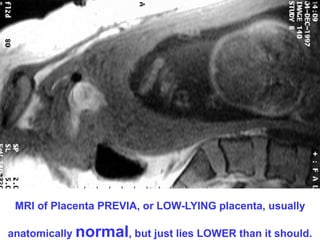
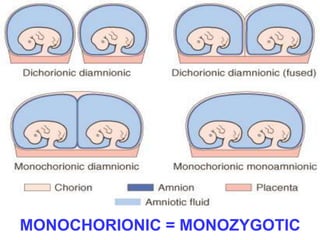
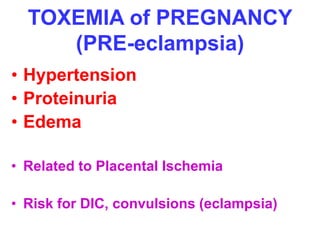
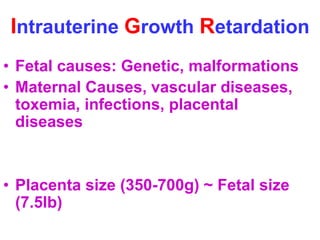
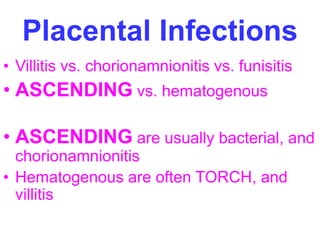
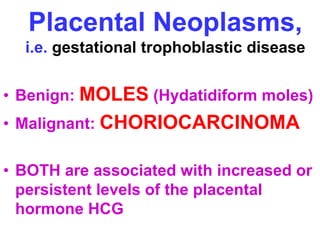
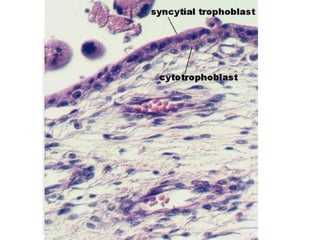
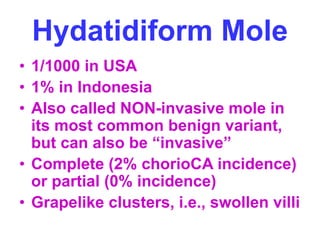
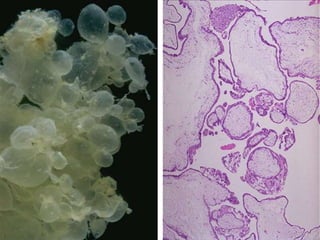
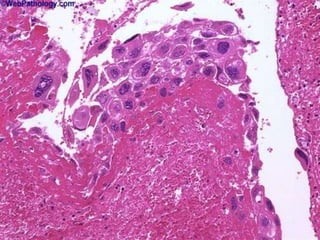
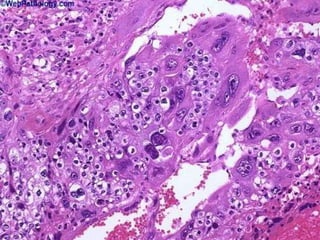
The document provides an overview of the female reproductive system, covering topics such as the vulva, vagina, cervix, uterus, fallopian tubes, ovaries, pregnancy, and placenta. Key points include common diseases and disorders that can affect each part of the reproductive system such as cysts, infections, inflammation, benign and malignant tumors. Early and late pregnancy complications are discussed as well as placental anomalies, infections, and rare tumors. Anatomical structures and terms are defined throughout.