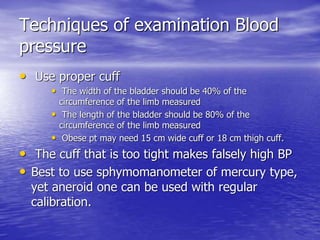
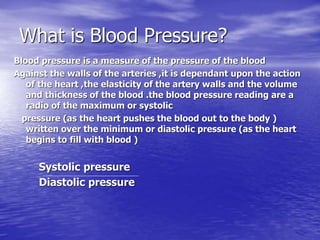
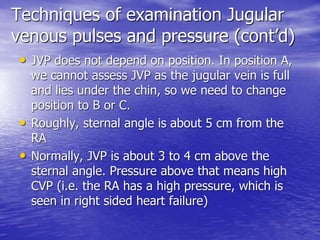
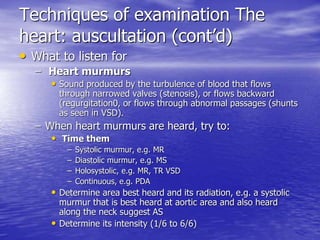
This document provides an outline and overview of techniques for performing a history and physical examination of the heart. It discusses the anatomy and physiology of the heart, techniques for examining pulses, heart sounds, murmurs, blood pressure, jugular veins, and special tests. The examination involves inspection, palpation, percussion, and auscultation of the heart and surrounding vessels to evaluate for abnormalities.