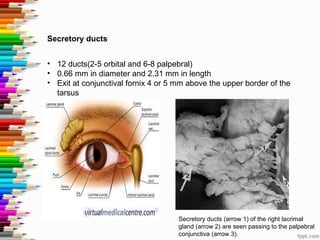
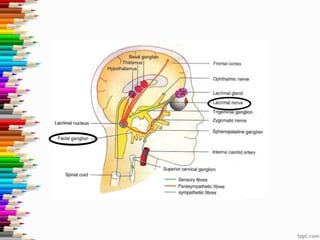
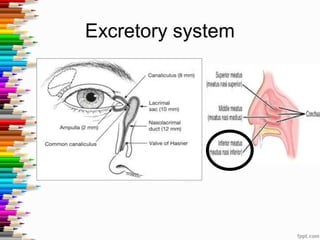
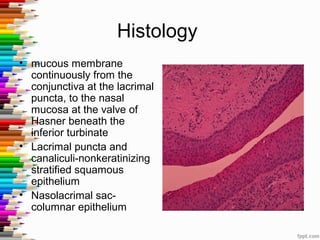
The document discusses the lacrimal system, including its embryology, anatomy, secretory and excretory systems, and physiology. It describes how the lacrimal system forms during embryonic development and can have congenital abnormalities. The key structures include the lacrimal gland, puncta, canaliculi, lacrimal sac, nasolacrimal duct, and associated valves. Tears are secreted and drained through coordinated contractions of the orbicularis oculi muscle and lacrimal pump mechanism to flush the eye surface and drain tears into the nasal cavity.