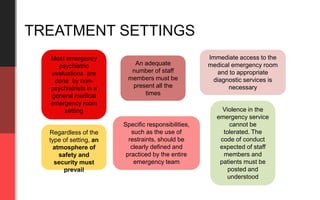
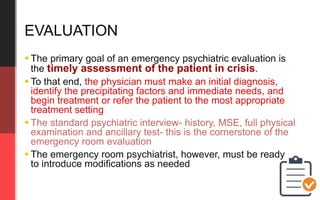
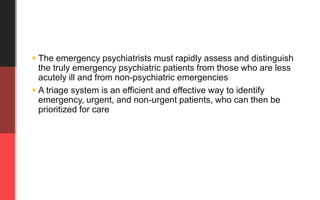
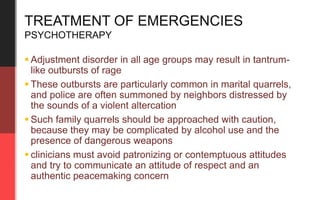
This document discusses evaluation and treatment settings and processes for emergency psychiatry. It notes that most emergency psychiatric evaluations are done in general emergency rooms by non-psychiatrists. It emphasizes the need for safety, security, adequate staffing, and clearly defined responsibilities in any treatment setting. The goals of evaluation are to make an initial diagnosis, identify precipitating factors and needs, and begin appropriate treatment or referral. Evaluation involves a standard psychiatric interview and potentially modified based on the emergency context. Treatment may involve psychotherapy, pharmacotherapy including sedation for violent patients, use of restraints in severe cases, and documentation of the evaluation, treatment, and disposition or referral of the patient.
![SITI MARIAM BINTI MOHD HAMZAH
Emergency Psychiatry
[Part 3] Evaluation & treatment](https://image.slidesharecdn.com/2-151217195447/85/2-emergency-psychiatry-1-320.jpg)