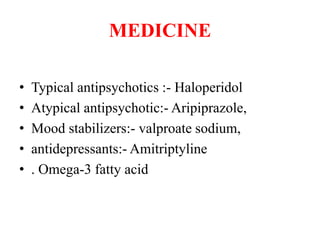
This document discusses borderline personality disorder (BPD). It defines BPD as a serious mental illness marked by unstable moods, behavior, and relationships. Common causes include genetic factors, childhood trauma, and stressful life events. Symptoms include fear of abandonment, unstable relationships, impulsivity, anger issues, and stress-related paranoia. BPD is diagnosed when 5 of 9 criteria are present for an extended period. Treatment involves counseling therapies like dialectical behavior therapy and medications. Nursing management focuses on safety, monitoring for destructive behaviors, encouraging social support, and setting clear behavioral boundaries.