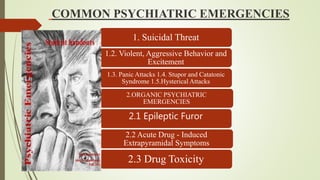
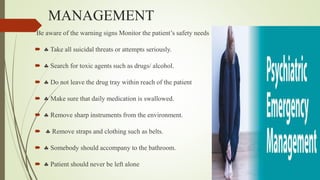
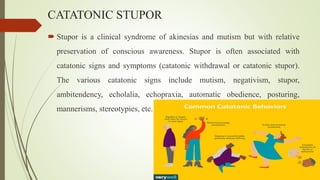
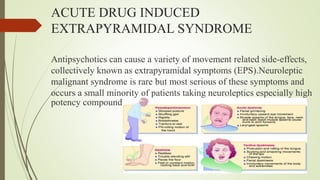
This document discusses various psychiatric emergencies and their management. It defines psychiatric emergency as a condition where a patient has disturbances in thought, affect, and psychomotor activity that threaten their existence or environment. Common emergencies discussed include suicidal threats, violent behavior, panic attacks, catatonic stupor, and hysterical attacks. Organic emergencies like epileptic furor and acute drug toxicity are also covered. For each emergency, risk factors, symptoms, and treatment approaches like reassurance, sedation, and removal from dangerous objects are summarized. The document stresses handling emergencies calmly to prevent anxiety in other patients.