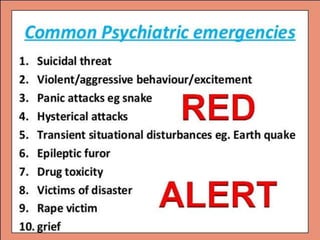
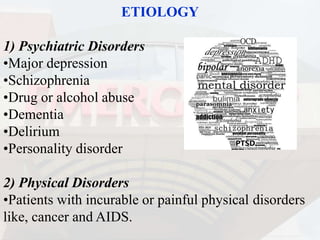
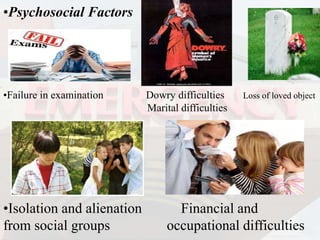
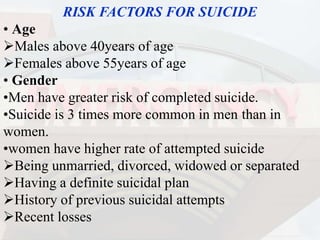
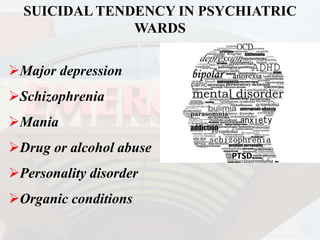
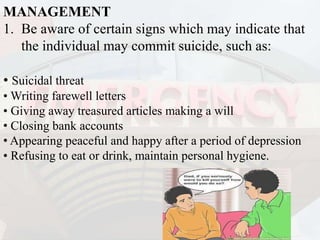
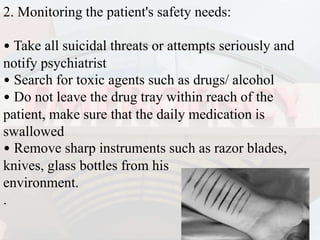
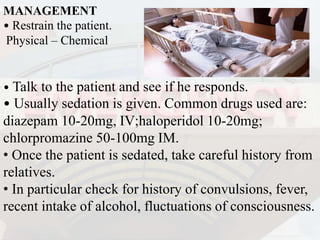
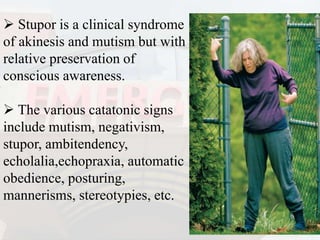
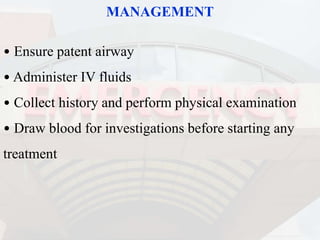
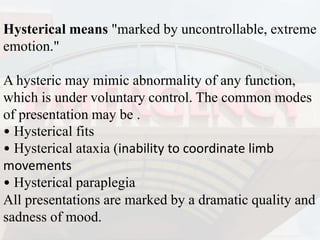
The document outlines psychiatric emergencies, defining them as acute behavioral changes that pose risks to patients and others. It covers various types of emergencies, including suicidal threats, violent behavior, and responses to panic attacks, along with their management strategies. The increasing prevalence of mental health issues necessitates that clinicians are well-informed about these emergencies to enhance patient care.