Panic disorder is characterized by unexpected panic attacks that occur without a discernible trigger. During attacks, patients feel an urge to flee and a sense of impending doom. Panic disorder is diagnosed based on the frequency and severity of panic attacks, as well as worry about future attacks. Treatment involves selective serotonin reuptake inhibitors (SSRIs), benzodiazepines, and cognitive-behavioral therapy, which are effective in more than 85% of cases. Long-term prognosis is generally good, with remission occurring within 6 months for 65% of patients.





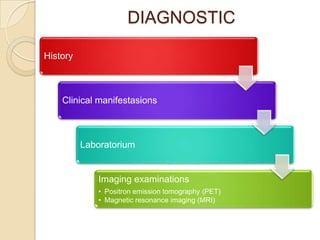
![Types of panic attacks
Unexpected panic attacks have no known precipitating cue;
these attacks often support the diagnosis of panic disorder
without agoraphobia.
Situationally predisposed panic attacks are more likely to occur
in relation to a given trigger, but they do not always occur. This
pattern more likely describes panic disorder with agoraphobia.
A variant of panic disorder unrelated to fear (nonfearful panic
disorder [NFPD]) is associated with high rates medical resource
use (32-41% of patients with panic disorder seeking treatment
for chest pain) and poor prognosis](https://image.slidesharecdn.com/panicdisorder-120523054712-phpapp02/85/Panic-disorder-7-320.jpg)
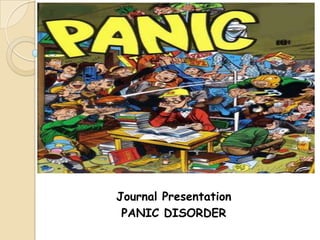
![Panic triggers
Triggers of panic can include the following:
• Injury (eg, accidents, surgery)
• Illness
• Interpersonal conflict or loss
• Use of cannabis (can be associated with panic attacks,
perhaps because of breath-holding)[5]
• Use of stimulants, such as caffeine, decongestants, cocaine,
and sympathomimetics (eg, amphetamine, MDMA)[6]
• Certain settings, such as stores and public transportation
(especially in patients with agoraphobia)
• Sertraline, which can induce panic in previously
asymptomatic patients[7]
• The selective serotonin reuptake inhibitor (SSRI)
discontinuation syndrome, which can induce symptoms
similar to those experienced by panic patients](https://image.slidesharecdn.com/panicdisorder-120523054712-phpapp02/85/Panic-disorder-8-320.jpg)