This document provides information on Campylobacter and Helicobacter, which are Gram-negative, microaerophilic bacteria. Campylobacter causes foodborne illness in humans and is transmitted through contaminated poultry or water. Its main virulence factors include flagella for motility and adhesins for attachment. Helicobacter pylori colonizes the stomach and is associated with gastritis, ulcers, and gastric cancer. It produces urease and adheres tightly to gastric epithelial cells using flagella and adhesins. Both bacteria are transmitted orally between humans or from animal reservoirs and cause disease by invading and damaging intestinal or gastric mucosa.
![Campylobacter 弯曲杆菌属 &
Helicobacte [hel 'k bæktə]ɪ ɒ 螺杆菌
rRNA Superfamily VI of Class Proteobacteria 变形杆
菌](https://image.slidesharecdn.com/12-campylobacterhelicobacter-150727150908-lva1-app6892/85/12-campylobacter-helicobacter-1-320.jpg)
![ Gram-negative
Helical (spiral or curved) morphology; Tend to be
pleomorphic
Characteristics that facilitate penetration and
colonization of mucosal environments (e.g.,
motile by polar flagella; corkscrew 螺丝锥 shape)
Microaerophilic atmospheric requirements
Become coccoid ['k k d]ɒ ɔɪ 球菌样的 when
exposed to oxygen or upon prolonged culture
Neither ferment nor oxidize[' ks da z]ɑː ɪ ɪ
carbohydrates
General Characteristics
Common to Superfamily](https://image.slidesharecdn.com/12-campylobacterhelicobacter-150727150908-lva1-app6892/85/12-campylobacter-helicobacter-2-320.jpg)
![ Distinctive rapid darting 飞镖 motility
• Long sheathed polar flagellum at one (polar)
or both (bipolar) ends of the cell
• Motility [mo 't lət ]ʊ ɪ ɪ slows quickly in wet mount
preparation
Microaerophilic & capnophilic[kæpnə'f l k]ɪ ɪ 嗜
二氧化碳的 ( 菌 ) 5%O2,10%CO2,85%N2
Thermophilic (42-43C) (except C. fetus)
• Body temperature of natural avian reservoir
May become nonculturable in nature](https://image.slidesharecdn.com/12-campylobacterhelicobacter-150727150908-lva1-app6892/85/12-campylobacter-helicobacter-5-320.jpg)
![Campylobacter Species Associated
with Human Disease
[pr k'ta t s]ɒ ɪ ɪ 传染性神经元炎
[ periə'd ntl]ˌ ɑː 牙周的
showae](https://image.slidesharecdn.com/12-campylobacterhelicobacter-150727150908-lva1-app6892/85/12-campylobacter-helicobacter-6-320.jpg)
![ Low incidence potential sequela [s 'kwi lə]ɪ ː 后遗症
Reactive, self-limited, autoimmune disease
Campylobacter jejuni most frequent antecedent
[ ænt 'si dnt]ˌ ɪ ː pathogen
Immune response to specific O-antigens cross-reacts
with ganglioside surface components of peripheral
nerves (molecular or antigenic mimicry)
• Acute inflammatory demyelinating [di 'ma ələ ne t]ː ɪ ˌ ɪ
neuropathy [n 'r pəθ ] (85% of cases) from crossʊ ɒ ɪ
reaction with Schwann-cells or myelin['ma əl n]ɪ ɪ 髓
磷脂 Acute axonal ['æks n]forms of GBS (15% ofɑː
cases) from molecular mimicry of axonal membrane
Guillain-Barre Syndrome (GBS)](https://image.slidesharecdn.com/12-campylobacterhelicobacter-150727150908-lva1-app6892/85/12-campylobacter-helicobacter-7-320.jpg)
![[m 'b dəti]ɔː ɪ](https://image.slidesharecdn.com/12-campylobacterhelicobacter-150727150908-lva1-app6892/85/12-campylobacter-helicobacter-11-320.jpg)
![ Infectious dose and host immunity determine
whether gastroenteric disease develops
• Some people infected with as few as 500 organisms
while others need >106
CFU
Pathogenesis not fully characterized
• No good animal model
• Damage (ulcerated, edematous and bloody) to the
mucosal surfaces of the jejunum [d 'd u nəm]ʒɪ ʒ ː ,
ileum[' liəm], colonɪ
• Inflammatory process consistent with invasion of the
organisms into the intestinal tissue; M-cell (Peyer’s
patches) uptake and presentation of antigen to
underlying lymphatic system
Non-motile & adhesin-lacking strains are avirulent
Pathogenesis & Immunity](https://image.slidesharecdn.com/12-campylobacterhelicobacter-150727150908-lva1-app6892/85/12-campylobacter-helicobacter-12-320.jpg)
![Cellular components:
Endotoxin
Flagellum [flə'd eləm]: Motilityʒ
Adhesins: Mediate attachment to mucosa
Invasins
GBS is associated with C. jejuni serogroup O19
S-layer protein “microcapsule” in C. fetus:
Extracellular components:
Enterotoxins
Cytopathic toxins
Putative ['pju tət v]Virulence Factorsː ɪ](https://image.slidesharecdn.com/12-campylobacterhelicobacter-150727150908-lva1-app6892/85/12-campylobacter-helicobacter-13-320.jpg)
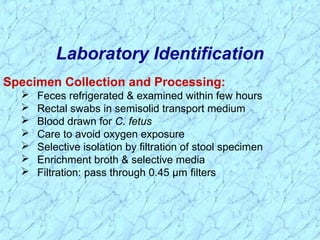
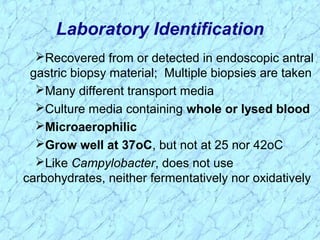
![Microscopy:
Gull-wing appearance in gram stain
Darting motility in fresh stool (rarely done in clinical lab)
Fecal leukocytes are commonly present
Identification:
Growth at 25o
, 37o
, or 42-43o
C
Hippurate ['h pj re t]ɪ ʊ ɪ 马尿酸盐 hydrolysis (C. jejuni is
positive)
Susceptibility to nalidixic acid 那利得酸 & cephalothin
['sefələθ n]ɪ 头孢菌素
Laboratory Identification](https://image.slidesharecdn.com/12-campylobacterhelicobacter-150727150908-lva1-app6892/85/12-campylobacter-helicobacter-15-320.jpg)
![Laboratory Identification (cont.)
[ n'd ks l]ɪ ɒ ɪ 吲羟 ['æs te t]ɪ ɪ 醋酸盐](https://image.slidesharecdn.com/12-campylobacterhelicobacter-150727150908-lva1-app6892/85/12-campylobacter-helicobacter-16-320.jpg)
![ Gastroenteritis:
•Self-limiting; Replace fluids and electrolytes
•Antibiotic treatment can shorten the excretion period;
Erythromycin is drug of choice for severe or complicated
enteritis & bacteremia; Fluroquinolones are highly active
(e.g., ciprofloxacin was becoming drug of choice) but
fluoroquinolone [fluərə kwa nə'lə n]resistanceʊ ɪ ʊ has
developed rapidly since the mid-1980s apparently related
to unrestricted use and the use of enrofloxacin
[enr f'l kse s n]ɒ ɒ ɪ ɪ 恩氟沙星 in poultry
•Azithromycin [e z θrə'ma s n]ɪ ɪ ɪ ɪ 阿奇霉素 was effective in
recent human clinical trials
•Control should be directed at domestic animal reservoirs
and interrupting transmission to humans
Treatment, Prevention & Control](https://image.slidesharecdn.com/12-campylobacterhelicobacter-150727150908-lva1-app6892/85/12-campylobacter-helicobacter-17-320.jpg)
![History & Taxonomy of Helicobacter
Family not yet named (17 species by rRNA sequencing)
First observed in 1983 as Campylobacter-like
organisms (formerly Campylobacter pyloridis) in the
stomachs of patients with type B
gastritis[ æ'stra t s]ɡ ɪ ɪ
Nomenclature [nə'menklət ər]ʃ 命名法 of
Helicobacter was first established in 1989, but only
three species are currently considered to be human
pathogens](https://image.slidesharecdn.com/12-campylobacterhelicobacter-150727150908-lva1-app6892/85/12-campylobacter-helicobacter-19-320.jpg)
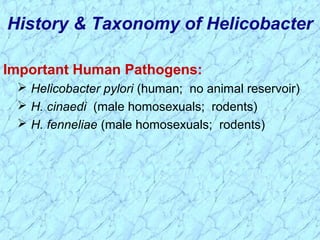
![ Helicobacter pylori is major human pathogen
associated with gastric antral ['æntrəm] 窦
epithelium in patients with active chronic gastritis
Stomach of many animal species also colonized
Urease (gastric strains only), mucinase, and
catalase positive highly motile microorganisms
Other Helicobacters: H. cinnaedi and H. fenneliae
• Colonize human intestinal tract
• Isolated from homosexual men with proctitis,
proctocolitis [pr k't kəla t s], enteritis, andɒ ɒ ɪ ɪ
bacteremia and are often transmitted through
sexual practices
General Characteristics of Helicobacter](https://image.slidesharecdn.com/12-campylobacterhelicobacter-150727150908-lva1-app6892/85/12-campylobacter-helicobacter-21-320.jpg)
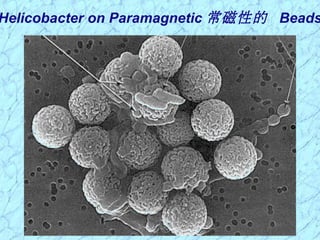
![ Gram-negative; Helical (spiral or curved) (0.5-1.0
um X 2.5-5.0 um); Blunted/rounded ends in gastric
biopsy specimens; Cells become rod-like and
coccoid on prolonged culture
Produce urease, mucinase, and catalase
H. pylori tuft [t ft]ʌ 一丛草 (lophotrichous
[ləfət'r t əs]ɪ ʃ ) of 4-6 sheathed flagella (30um X
2.5nm) attached at one pole
Single polar flagellum on H. fennellae & H. cinaedi
Smooth cell wall with unusual fatty acids
Morphology & Physiology of
Helicobacter](https://image.slidesharecdn.com/12-campylobacterhelicobacter-150727150908-lva1-app6892/85/12-campylobacter-helicobacter-22-320.jpg)
![Helicobacter Species Associated
with Human Disease
消化的
犬属
['p lərəm]ʊ 鸡白色腹泻
[ræ'pi n ]ː ɪ 嫩芜青
卡纳登西斯](https://image.slidesharecdn.com/12-campylobacterhelicobacter-150727150908-lva1-app6892/85/12-campylobacter-helicobacter-24-320.jpg)
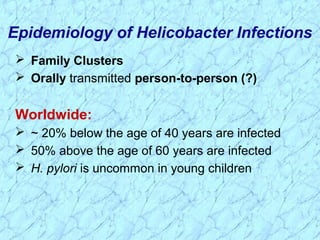
![Developed Countries:
United States: 30% of total population infected
• Of those, ~1% per year develop duodenal
[ dju ə'di nl]ˌ ː ː ulcer
• ~1/3 eventually have peptic ulcer disease(PUD)
70% gastric ulcer cases colonized with H. pylori
Low socioeconomic status predicts H. pylori infection
Epidemiology of Helicobacter Infections (cont.)](https://image.slidesharecdn.com/12-campylobacterhelicobacter-150727150908-lva1-app6892/85/12-campylobacter-helicobacter-26-320.jpg)
![ Colonize mucosal lining of stomach & duodenum
in man & animals
• Adherent to gastric surface epithelium or pit epithelial cells
deep within the mucosal crypts 腺窝 adjacent to gastric
mucosal cells
• Mucosa protects the stomach wall from its own gastric
milieu [mi 'lj ]ː ɜː 周围环境 of digestive enzymes and
hydrochloric acid
• Mucosa also protects Helicobacter from immune response
Most gastric adenocarcinomas 肺鳞癌 and
lymphomas are concurrent with or preceded by an
infection with H. pylori
Pathogenesis of Helicobacter Infections](https://image.slidesharecdn.com/12-campylobacterhelicobacter-150727150908-lva1-app6892/85/12-campylobacter-helicobacter-28-320.jpg)
![Virulence Factors of Helicobacter
[ ha pəklo r'ha dr ə]ˌ ɪ ʊ ɪ ɪ 胃酸过少 [pə'ra ətəl]ɪ 腔壁的](https://image.slidesharecdn.com/12-campylobacterhelicobacter-150727150908-lva1-app6892/85/12-campylobacter-helicobacter-29-320.jpg)
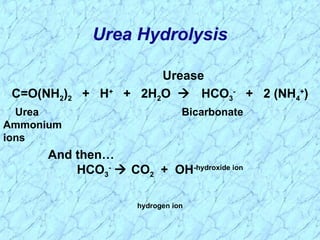
![ Multiple polar, sheathed flagella
• Corkscrew motility enables penetration into
viscous['v skəs] environment (mucus)ɪ
Adhesins: Hemagglutinins; Sialic acid binding
adhesin; Lewis blood group adhesin
Mucinase: Degrades gastric mucus; Localized
tissue damage
Urease converts urea (abundant in saliva and
gastric juices [d u s]) into bicarbonate (to COʒ ː 2) and
ammonia
• Neutralize the local acid environment
• Localized tissue damage
Acid-inhibitory protein
Virulence Factors of Helicobacter](https://image.slidesharecdn.com/12-campylobacterhelicobacter-150727150908-lva1-app6892/85/12-campylobacter-helicobacter-30-320.jpg)

![Triple Chemotherapy (synergism
['s nəd zm]):ɪ ʒɪ
Proton['pro t n]ʊ ɑː 质子 pump inhibitor (e.g.,
omeprazole [o 'meprə zo l]ʊ ˌ ʊ 奥美拉唑 = Prilosec(R))
One or more antibiotics (e.g.,
clarithromycin[klær θrə'ma s n]ɪ ɪ ɪ 克拉霉素 ; amoxicillin
[əm ks 's l n]ɒ ɪ ɪ ɪ 阿莫西林 ; metronidazole[ metrə'na dəˌ ɪ
zo l]ˌ ʊ 灭滴灵 )
Bismuth['b zməθ]ɪ 铋 compound
Inadequate treatment results in recurrence of symptoms
Treatment, Prevention & Control](https://image.slidesharecdn.com/12-campylobacterhelicobacter-150727150908-lva1-app6892/85/12-campylobacter-helicobacter-34-320.jpg)