The document discusses lung cancer, including:
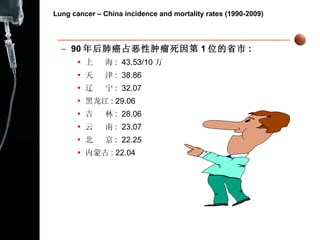
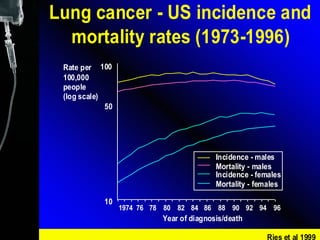
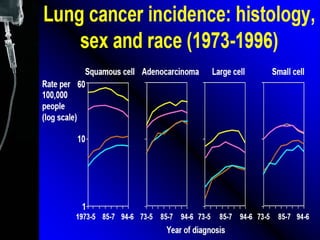
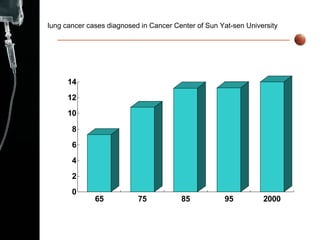
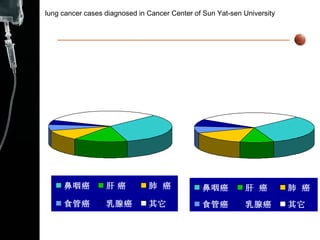
1) Lung cancer incidence and mortality rates have increased in China since 1990, becoming the leading cause of cancer death.
2) Risk factors for lung cancer include cigarette smoking, air pollution, certain occupations, and genetic factors.
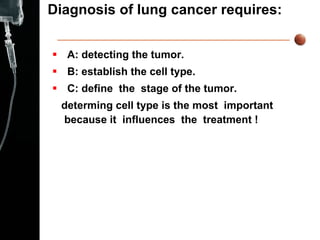
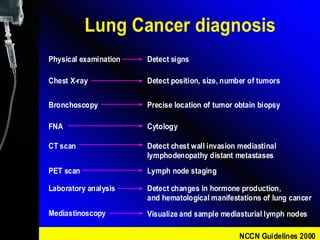
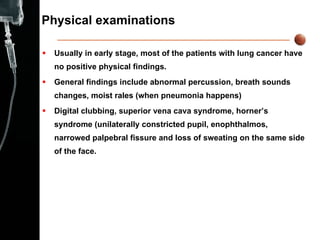
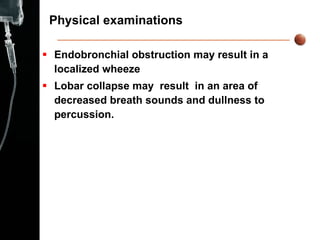
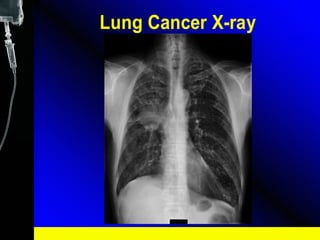
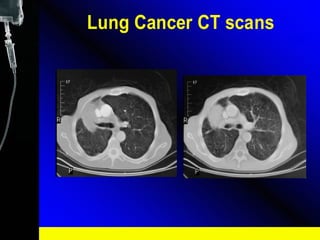
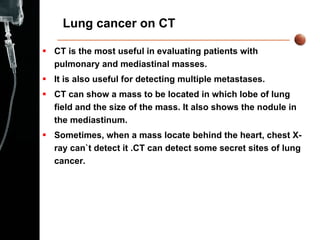
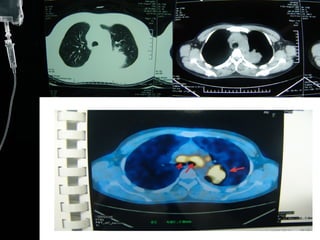
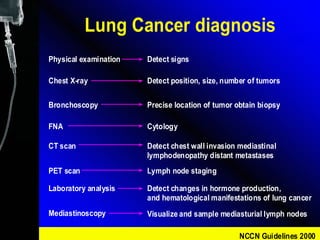
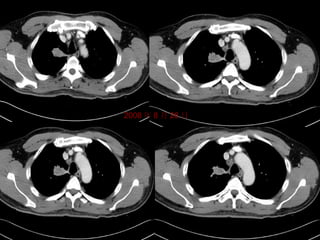
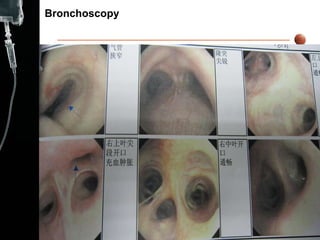
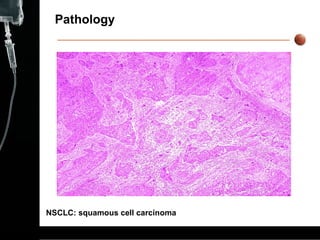
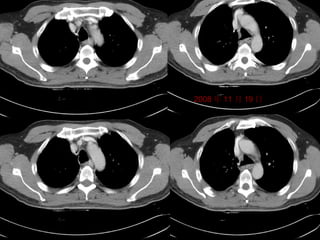
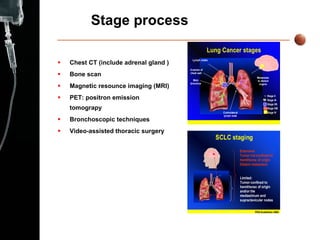
3) Diagnosis involves imaging like chest X-rays and CT scans, as well as procedures like bronchoscopy to obtain tissue samples.
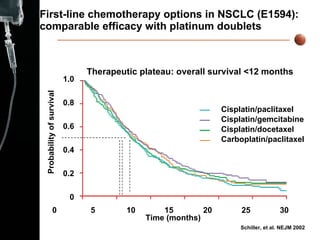
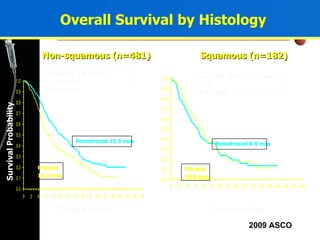
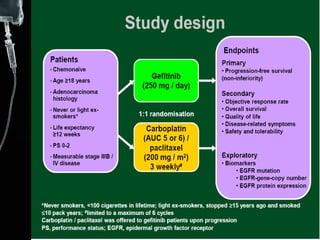
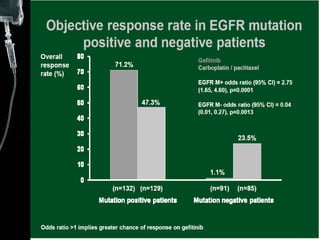
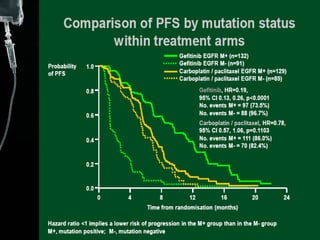
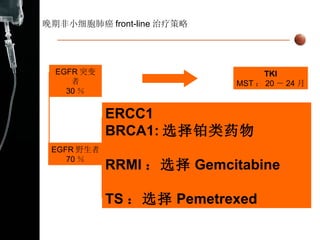
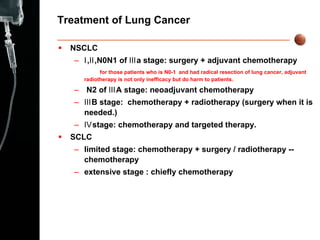
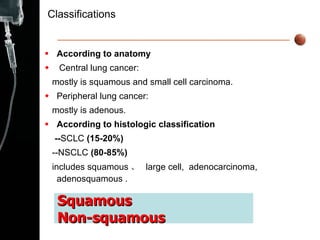
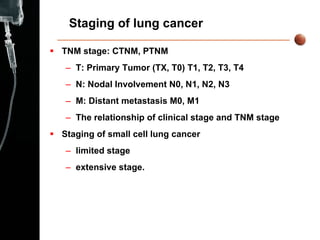
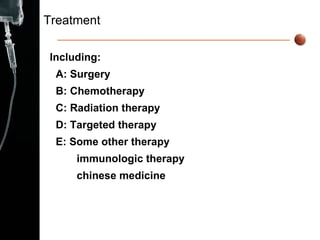
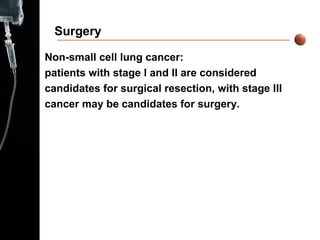
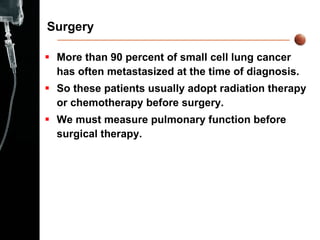
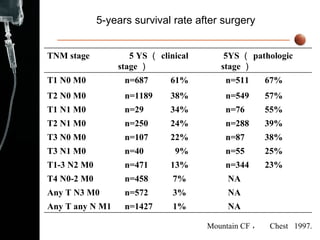
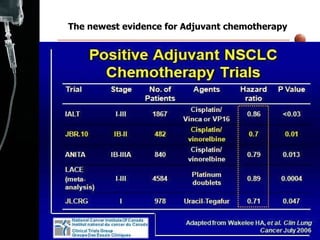
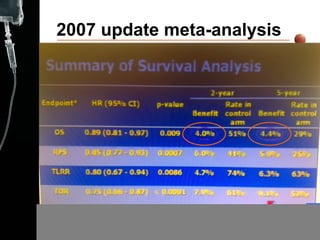
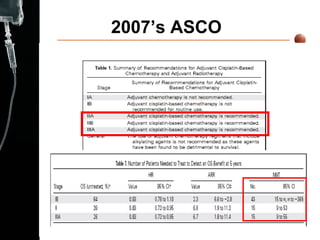
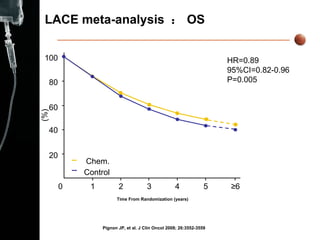
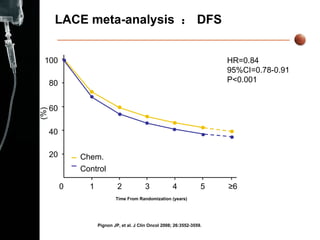
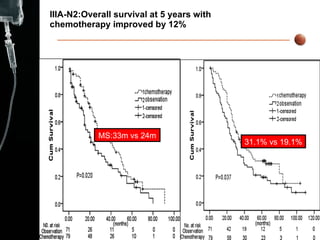
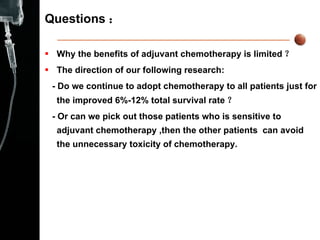
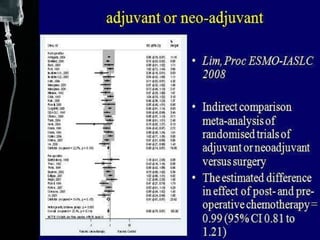
4) Treatment depends on cancer type and stage, and may involve surgery, chemotherapy, radiation therapy, targeted therapy, and other approaches. Adjuvant chemotherapy provides a limited survival benefit for non-small cell lung cancer.

![LACE meta-analysis : Survival according to type of death. Decreases lung cancer–related death (HR=0.83, 95%CI=0.76-0.90, P<0.001) Increase noncancer-related death (HR=1.36, 95%CI=1.10-1.69, P=0.004) 主要出现在前 6 个月 (HR=2.41, 95%CI=1.64-3.55, P<0.001) Pignon JP, et al. J Clin Oncol 2008; 26:3552-3559.[ 临床肿瘤学杂志中文版 2009; 3(1): 10-17.] 100 80 60 40 20 0 1 2 3 4 5 ≥ 6 Time From Randomization (years) Survival (%) Chem. ( noncancer-related death ) Cont (noncancer-related death ) 化疗 ( 癌症相关死亡 ) 不化疗 ( 癌症相关死亡 )](https://image.slidesharecdn.com/10lungcancer-100420053919-phpapp01/85/10-lung-cancer-47-320.jpg)
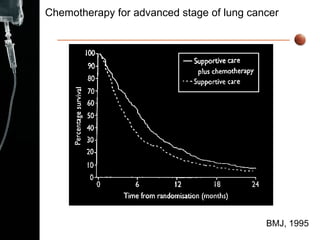
![NSCLC Meta-analyses NSCLC Meta-analyses Collaborative Group. JCO 2008; 26:4617-25 .[ 临床肿瘤学杂志中文版 2009; 3(2): 45.] 16 项 RCT 2714 例患者 IPD 资料 HR=0.77 95%CI=0.71-0.83 P≤0.0001 1YS: 29% vs. 20% 1.0 0.8 0.6 0.4 0.2 0 3 6 9 12 15 18 21 24 时间 ( 月 ) 概率 事件数 患者总数 1240 1293 1315 1399 SC+CT 仅 SC](https://image.slidesharecdn.com/10lungcancer-100420053919-phpapp01/85/10-lung-cancer-53-320.jpg)