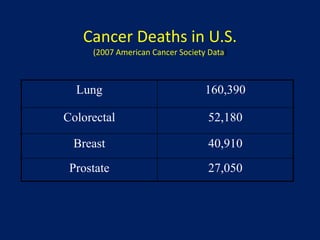
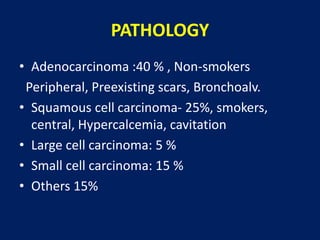
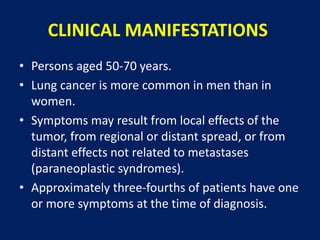
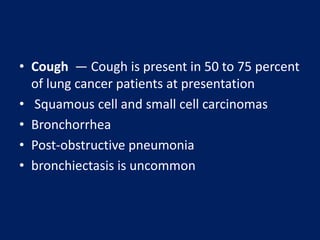
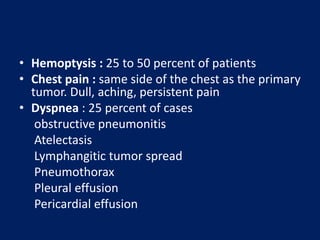
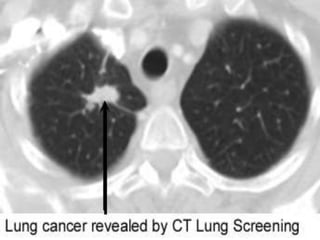
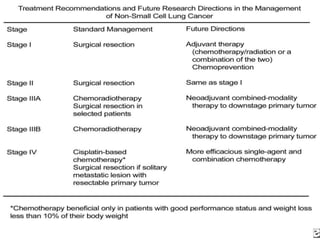
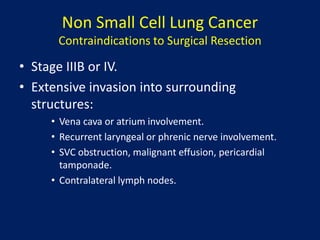
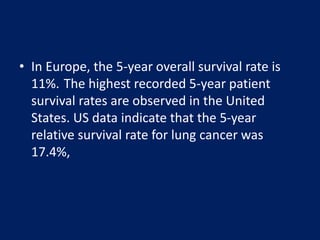
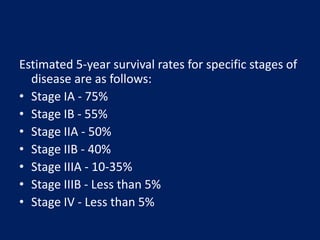
Lung cancer is the leading cause of cancer death worldwide. Smoking is responsible for about 90% of lung cancer cases. The risk of lung cancer is greatly increased in current or former smokers. Screening with low-dose CT is recommended for those aged 55-80 with a significant smoking history. The main types of lung cancer are small cell lung cancer and non-small cell lung cancer. Symptoms vary depending on the location and size of the tumor but may include cough, hemoptysis, chest pain, and weight loss. Treatment options include surgery, chemotherapy, and radiation therapy. Prognosis depends on the stage of cancer at diagnosis.