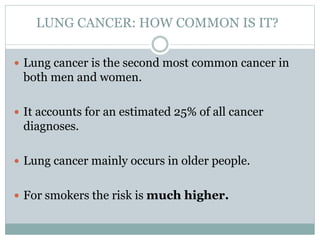
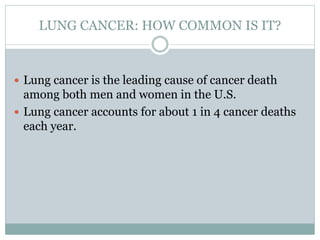
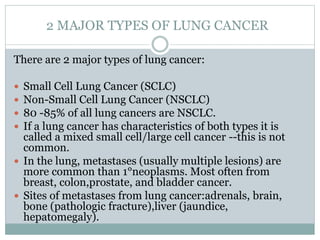
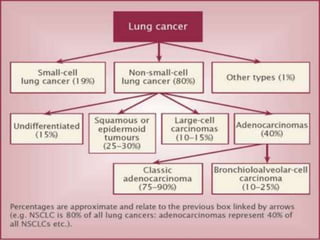
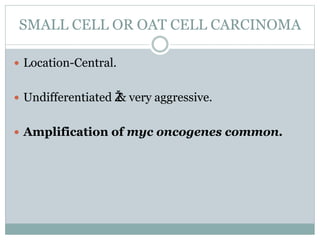
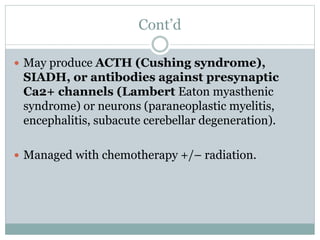
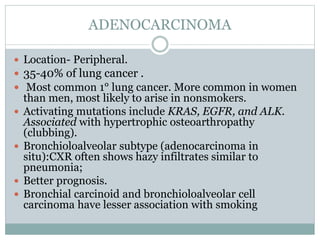
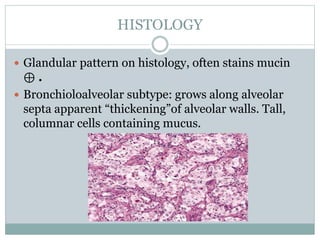
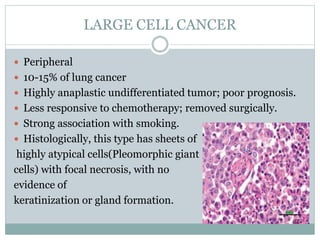
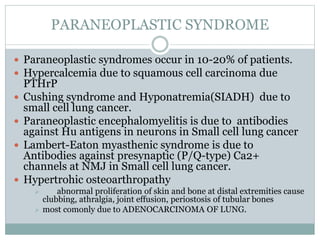
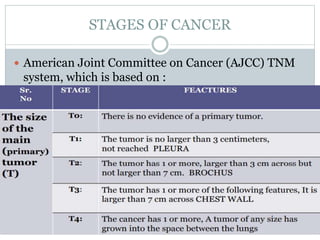
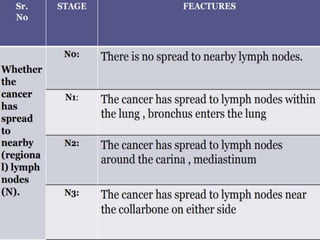
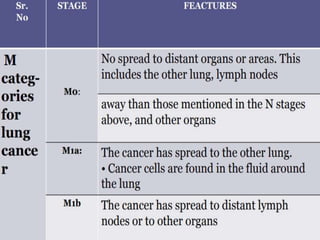
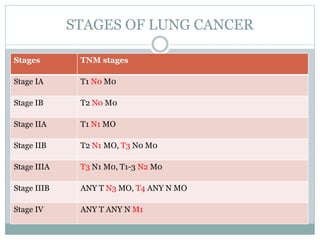
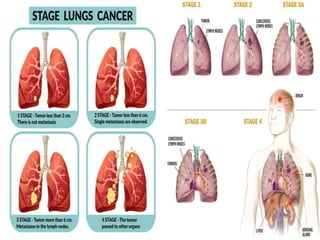
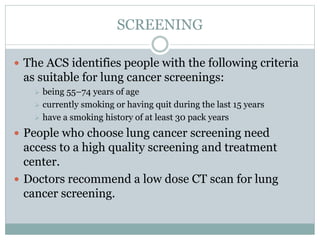
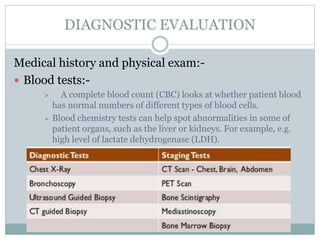
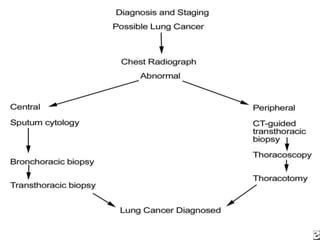
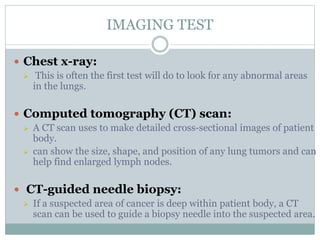
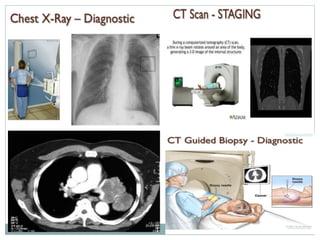
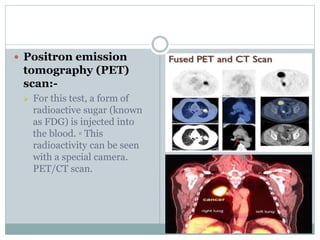
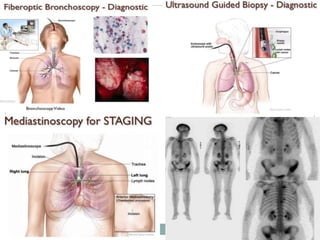
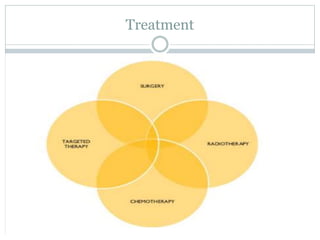
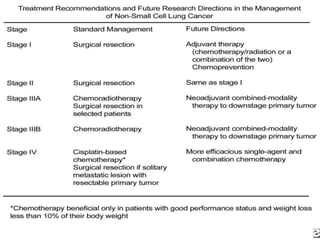
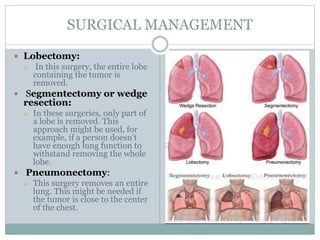
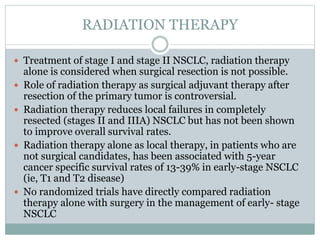
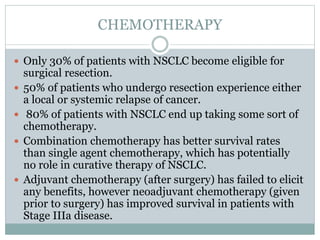
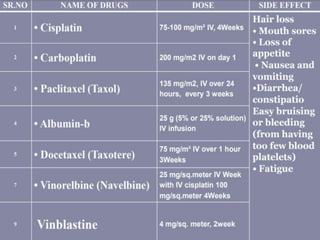
Lung cancer is a leading cause of cancer death. It is often caused by smoking and affects the lungs and other organs. The main types are small cell lung cancer and non-small cell lung cancer (which includes adenocarcinoma, squamous cell carcinoma, and large cell carcinoma). Symptoms include cough, chest pain, and weight loss. Screening is recommended for older adults with a significant smoking history. Treatment involves surgery, chemotherapy, radiation therapy, and targeted drug therapies depending on cancer type and stage. The goal is early detection and treatment to improve outcomes.