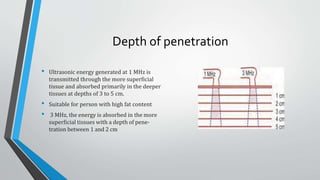
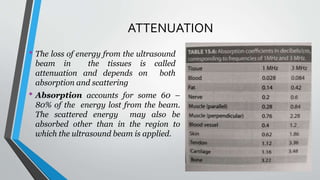
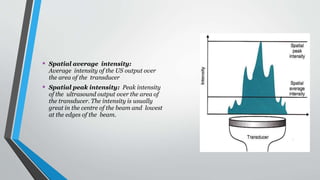
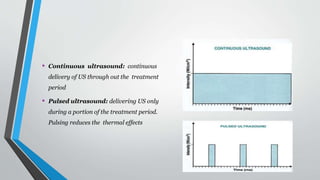
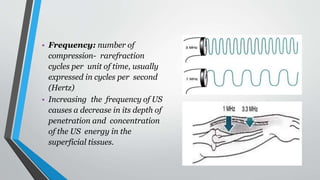
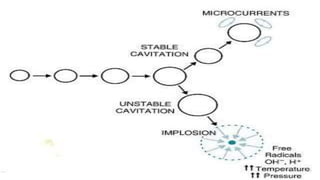
Ultrasound therapy uses high frequency sound waves to generate heat deep in tissues for therapeutic purposes. A generator sets the ultrasound frequency between 1-3 MHz, with higher frequencies penetrating less deeply. Pulsed ultrasound is safer as it allows time for heat to dissipate between pulses. Non-thermal effects include cavitation, acoustic streaming, and micromassage. Ultrasound promotes healing in acute injuries by stimulating inflammatory responses and collagen synthesis. It helps remodel scar tissue and accelerate wound healing in chronic injuries by increasing membrane permeability. Common uses are for varicose ulcers, pressure sores, pain relief in herpes zoster and back pain. Moving the transducer head prevents heat build up and damage from standing waves.