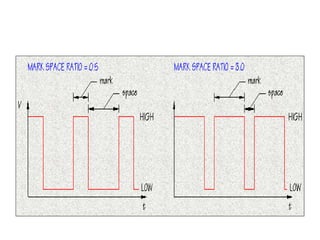
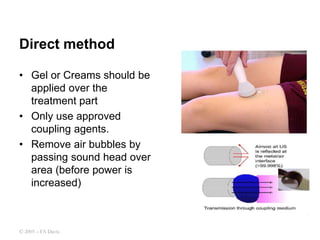
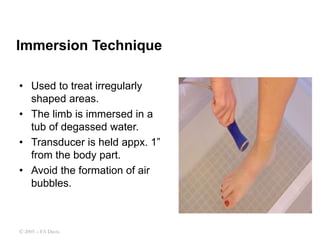
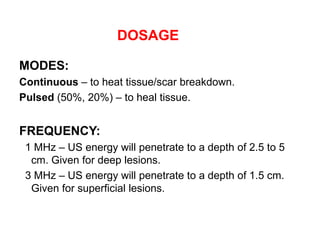
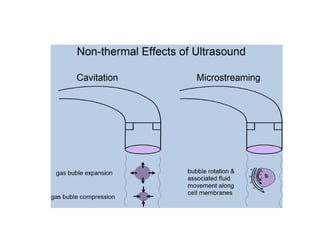
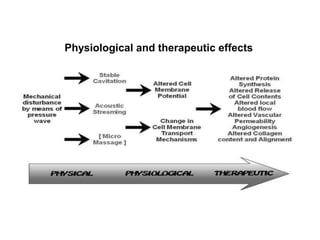
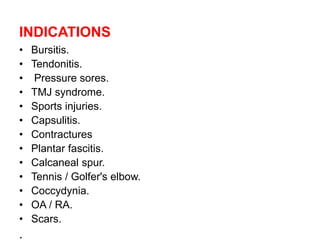
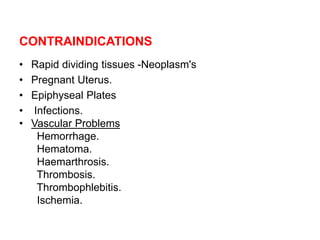
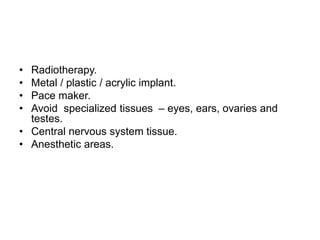
This document discusses therapeutic ultrasound. It defines ultrasound as acoustic vibrations too high for human hearing between 0.5-5 MHz. It describes ultrasound parameters like intensity, duration, and mark-space ratio. It discusses continuous and pulsed wave types and dosage considerations. Application methods like direct contact, immersion, and pads are covered. Physiological effects include increased blood flow and permeability. Indications include injuries while contraindications involve cancers or implants. Precautions to avoid burns are described.