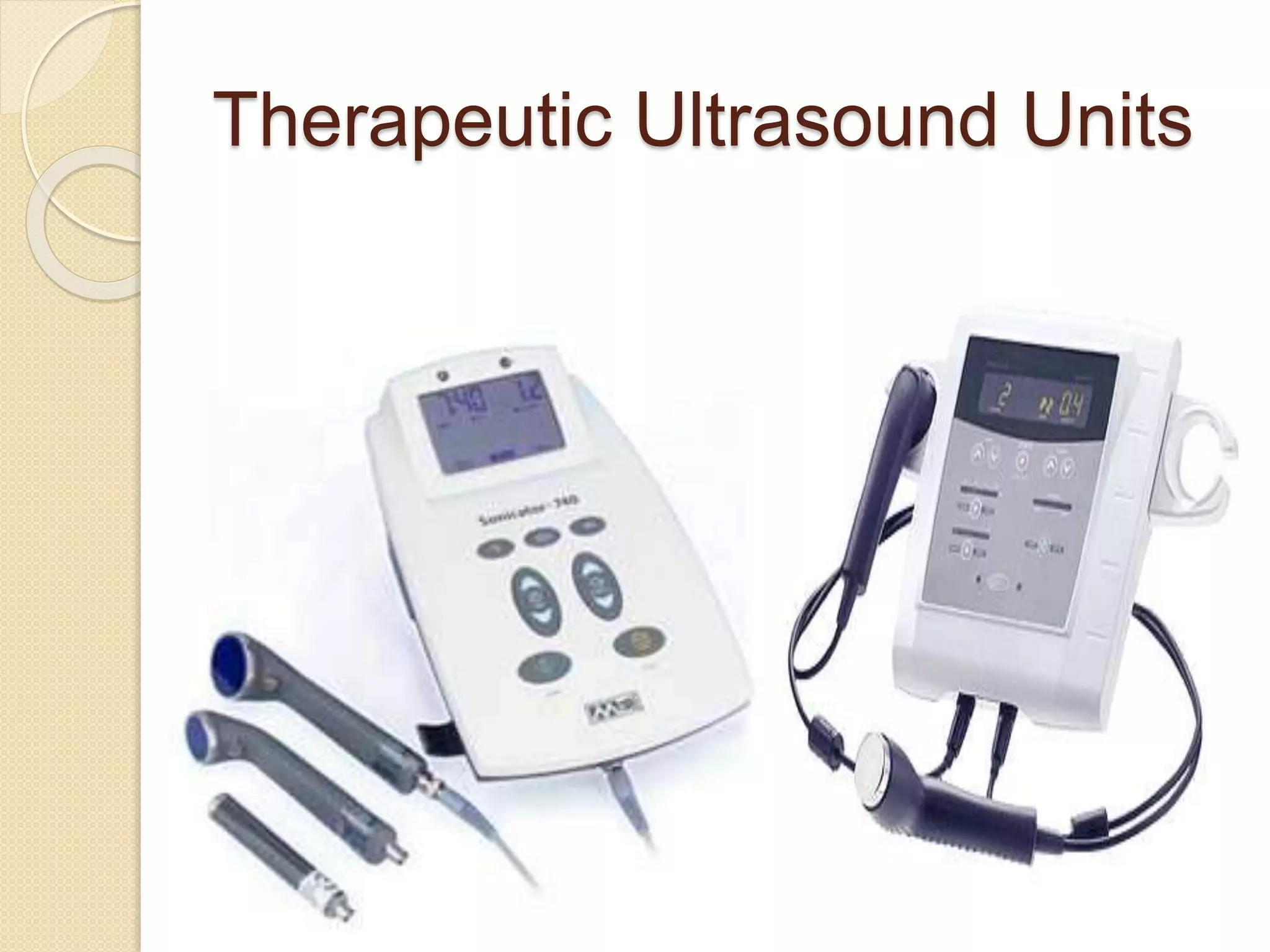
This document discusses therapeutic ultrasound including its physical principles, biophysical effects, clinical applications, and guidelines for safe use. Ultrasound uses piezoelectric crystals to generate sound waves that can be used for imaging, physical therapy, and tissue destruction. Its effects include increased tissue temperature, cavitation, and mechanical alterations. Common uses are for joint contractures, pain/spasm, tendinitis, and wound healing. Guidelines cover intensity, duration, frequency selection, and precautions to avoid harm. Case studies demonstrate ultrasound for various conditions.