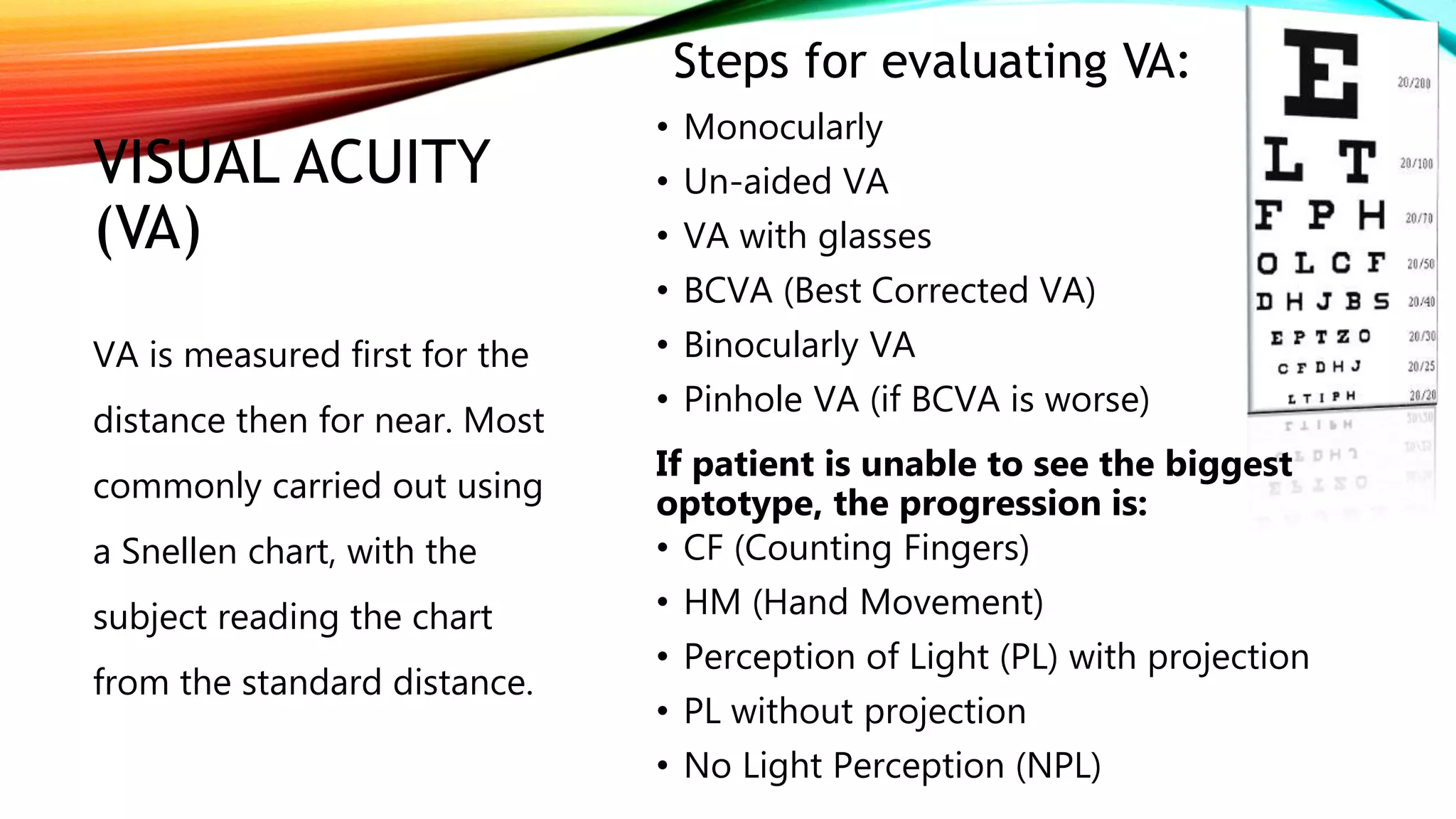
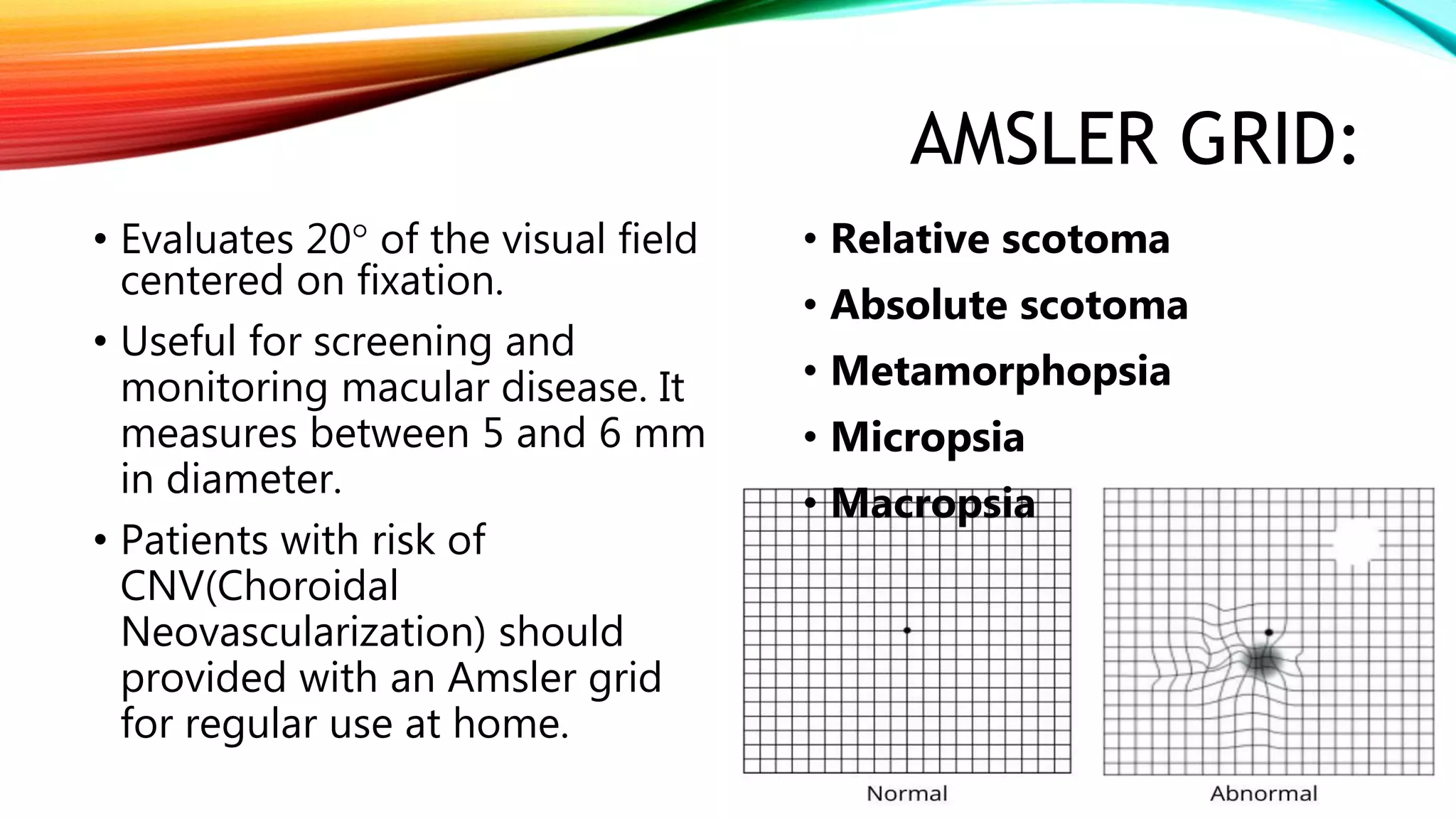
The document outlines various methods for eye examination, including external examination, visual acuity assessment, color vision testing, and more. Each method is described in detail along with the tools and techniques used for the evaluation. The document serves as a comprehensive guide for ophthalmic examinations, highlighting essential assessments such as pupillary reaction, extraocular motility, and advanced diagnostic tools like tonometry and gonioscopy.