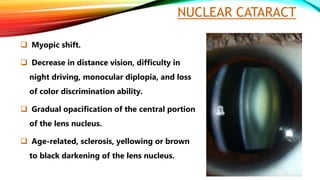
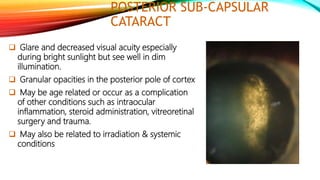
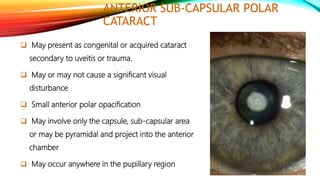
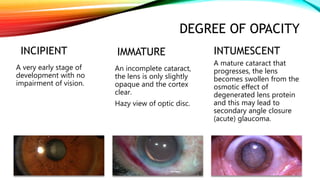
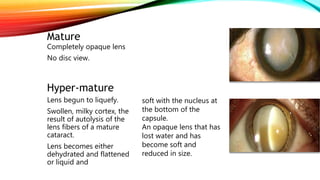
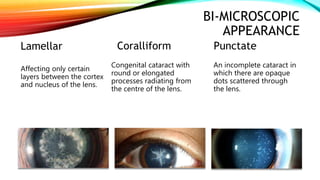
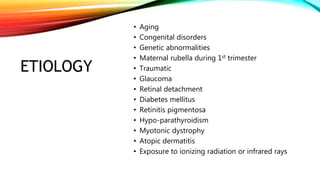
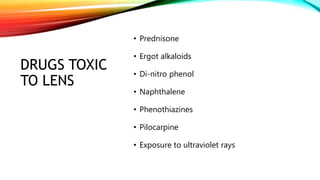
Cataract is a cloudiness or opacity of the normally transparent crystalline lens of the eye that can cause decreased vision and eventual blindness. Cataracts can be classified in several ways, including by their location in the lens, the age of onset, the degree of opacity, and their appearance during examination. The most common types are nuclear cataracts, which involve the central lens nucleus, and cortical cataracts, which start as water clefts and vacuoles in the lens cortex. Cataracts can develop due to aging, congenital issues, genetic factors, trauma, diabetes, medications, radiation exposure, and other medical conditions.