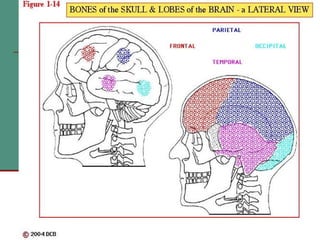
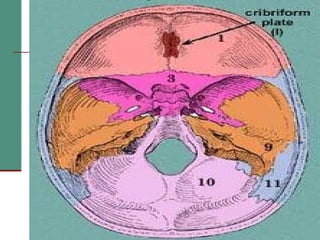
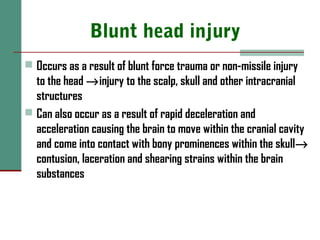
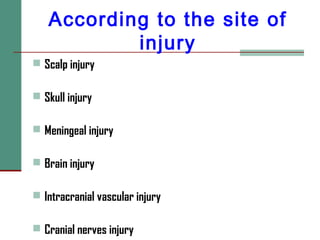
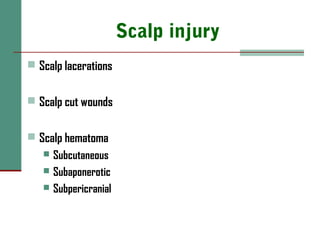
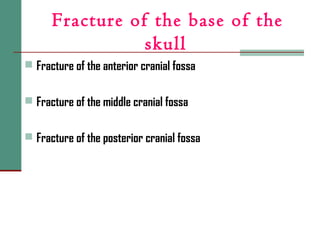
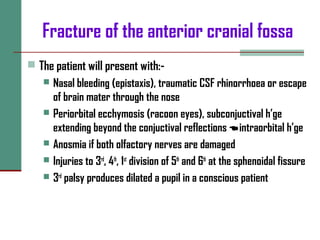
This document provides an overview of head injuries, including definitions, surgical anatomy of relevant structures like the scalp, skull, meninges and brain, epidemiology, etiology, classifications, pathophysiology, clinical presentation, workup and management. It discusses different types of head injuries such as blunt and penetrating injuries, and classifications based on integrity of the dura mater, site of injury and pathology. Specific types of injuries like fractures, hematomas, and brain injuries are described in detail.
![HEAD INJURIES
Dr Phillipo L. Chalya M.D. ;M.Med [Surg]
Surgeon specialist
Dept of Surgery
BMC](https://image.slidesharecdn.com/01-150427073911-conversion-gate01/85/01-head-injuries-dr-phillip-bmc-1-320.jpg)
![Scalp
Skin
Thick, hair bearing with many
sebaceous glands
Connective tissue
Fibro-fatty
Many blood vessels
Aponeurosis [epicranial]
Tough structure joining occipitalis
muscle posteriorly and frontalis
anteriorly
Loose areola tissue
Occupies the subaponeurotic space
Pericranium
Periosteum covering the outer
surface of the skull](https://image.slidesharecdn.com/01-150427073911-conversion-gate01/85/01-head-injuries-dr-phillip-bmc-6-320.jpg)
![Skull
22 bones in total
Consists of:-
8 cranial bones [cranium]
14 facial bones
Cranium is that part of the skull that encloses the brain
The cranium is made up of the vault [the upper part] and the base
of the skull [lower part]
The inner aspect of the base of the skull consists of 3 cranial
fossae:-
Anterior cranial fossa
Middle cranial fossa
Posterior cranial fossa](https://image.slidesharecdn.com/01-150427073911-conversion-gate01/85/01-head-injuries-dr-phillip-bmc-7-320.jpg)
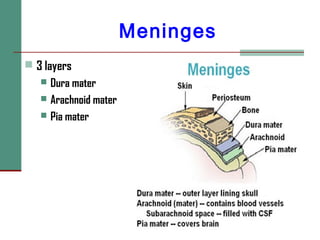
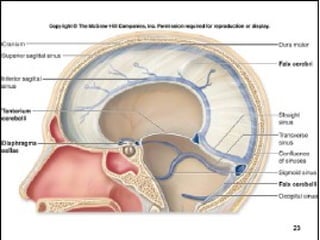
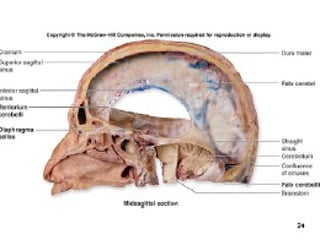
![Dura mater
Conventionally 2 layers:
Endosteal layer (periosteum)
Meningeal layer (true dura)
Septa: made up of dural folds
Divides the cranial cavity into 3 compartments
2 upper compartments [supratentorial compartments]
1 lower compartment [infratentorial compartment]
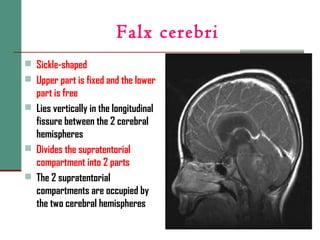
Major dural folds include:-
Falx cerebri
Tentorium cerebelli](https://image.slidesharecdn.com/01-150427073911-conversion-gate01/85/01-head-injuries-dr-phillip-bmc-11-320.jpg)
![Tentorium cerebelli
Crescent shaped
Lies horizontally between the occipital lobe of the cerebrum and
the cerebellum
Posteriorly is fixed
Anteriorly is free with an opening [tentorial notch] for passage of
the midbrain
Has a protective function
it prevents shuddering movements of the brain within the cranial
cavity and the folds prevent damage to nervous tissue during
sudden rotational movements](https://image.slidesharecdn.com/01-150427073911-conversion-gate01/85/01-head-injuries-dr-phillip-bmc-14-320.jpg)
![sex
Males are more affected than females
The male to female ratio is 2:1 [M:F= 2:1] worldwide](https://image.slidesharecdn.com/01-150427073911-conversion-gate01/85/01-head-injuries-dr-phillip-bmc-28-320.jpg)
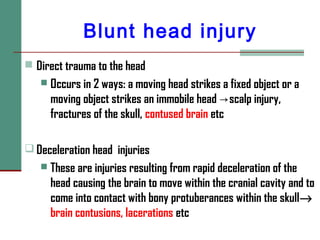
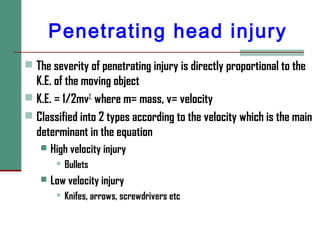
![According to mechanism
of injury
Blunt head injury [Non-missile injuries]
Penetrating head injury [Missile injuries]](https://image.slidesharecdn.com/01-150427073911-conversion-gate01/85/01-head-injuries-dr-phillip-bmc-34-320.jpg)
![Skull injury
Fracture of the vault [vault skull fracture]
Fracture of the base of the skull [basilar fracture]](https://image.slidesharecdn.com/01-150427073911-conversion-gate01/85/01-head-injuries-dr-phillip-bmc-42-320.jpg)
![Fracture of the vault
According to whether the fracture is exposed to the outside world
Simple [closed] fracture: The fracture is not exposed the outside
Compound [open] fracture : The fracture is exposed to the outside
According to the type of fracture
Liner fracture
Depressed fracture
Comminuted fracture](https://image.slidesharecdn.com/01-150427073911-conversion-gate01/85/01-head-injuries-dr-phillip-bmc-43-320.jpg)
![Fracture of the middle cranial fossa
This presents with:-
Bleeding from the ears [hemotympanum] or mouth
CSF otorrhoea
CSF Rhinorrhoea via the eustachian tube
Oscular disruption
7th
and 8th
cranial nerve palsies →facial palsy and deafness
respectively](https://image.slidesharecdn.com/01-150427073911-conversion-gate01/85/01-head-injuries-dr-phillip-bmc-46-320.jpg)
![Fracture of the posterior cranial fossa
Extravasation of blood may be seen in the suboccipal region
producing a swelling at the back
Post auricular [posterior to the mastoid process] ecchymosis
[Battle’s sign]
Injury to the 9th
, 10th
and 11st at the jugular foramen](https://image.slidesharecdn.com/01-150427073911-conversion-gate01/85/01-head-injuries-dr-phillip-bmc-47-320.jpg)
![Cerebral laceration
In this condition the brain surface is torn with effusion of blood
into CSF→SAH [subarachnoid h’ge]
This occurs when there is a significant force to the skull
→laceration of the brain as a result of rapid movement and
shearing of brain tissue
The pia mater and arachnoid may be torn →ICH [intra-cerebral
h’ge]
Focal neurological deficits are common
Clinically presents as cerebral contusion](https://image.slidesharecdn.com/01-150427073911-conversion-gate01/85/01-head-injuries-dr-phillip-bmc-53-320.jpg)
![Subarachnoid haematoma
Haematoma in the space between the arachnoid space and the pia
mater [subarachnoid space]
Occurs when a vessel ruptures into the subarachnoid layer or in
case of cerebral lacerations
There is extravasations of blood under pressure into the CSF
space, ventricles or into the brain itself
The patient presents with severe headache of sudden onset,
nausea and vomiting](https://image.slidesharecdn.com/01-150427073911-conversion-gate01/85/01-head-injuries-dr-phillip-bmc-59-320.jpg)
![According to severity
Classified according to Glasgow Coma Score [GCS]
Classified into:-
Mild head injury [GCS of 13-15]
Moderate head injury [GCS of 9-12]
Severe head injury [ GCS of 3-8 ]](https://image.slidesharecdn.com/01-150427073911-conversion-gate01/85/01-head-injuries-dr-phillip-bmc-65-320.jpg)
![PATHOPHYSIOLOGY
Requires understanding of the following crucial concepts:-
The concept of Monro-Kellie doctrine
The concept of Cerebral Perfusion Pressure [CPP]
The concept of increased ICP](https://image.slidesharecdn.com/01-150427073911-conversion-gate01/85/01-head-injuries-dr-phillip-bmc-66-320.jpg)
![Monro-Kellie doctrine
The skull is a rigid structure (once the sutures have fused)
3 components within that have a balance
80% brain
10% blood
10% CSF
If any one of these components increases [or if there is a SOL]
another component must decrease to maintain the balance (ICP)
If this does not happen then there will be an increase in ICP
This observations were first reported by Monro [1783] and
confirmed by Kellie 40 years later→ becoming known as the
Monro-Kellie docrine](https://image.slidesharecdn.com/01-150427073911-conversion-gate01/85/01-head-injuries-dr-phillip-bmc-67-320.jpg)
![Cerebral Perfusion
Pressure [CPP]
CPP is defined as the difference between the mean arterial
pressure (MAP) and the ICP [ i.e. CPP = MAP – ICP]
CPP is the net pressure required to deliver blood to the brain
Cerebral blood flow (CBF) is constant in the range of MAPs of 50-
150 mm Hg
This is due to autoregulation by the arterioles
As ICP increases, in order to maintain a constant CPP there has to
be a compensatory rise in the MAP
A hypertensive response is therefore elicited which classically is
associated with bradycardia
This is termed as the Cushing reflex after the eminent American
neurosurgeon](https://image.slidesharecdn.com/01-150427073911-conversion-gate01/85/01-head-injuries-dr-phillip-bmc-68-320.jpg)
![Cerebellar herniation
2 types:-
Upward cerebellar herniation
Downward cerebellar herniation [tonsillar]](https://image.slidesharecdn.com/01-150427073911-conversion-gate01/85/01-head-injuries-dr-phillip-bmc-74-320.jpg)
![Cerebral ischaemia
ICP results in CPP and therefore CBF [CPP= MAP-ICP]→
cerebral ischaemia
This is common after severe head injury and is caused by a
combination of either hypoxia and impaired cerebral
perfusion
The brain is unable to autoregulate its blood supply with a
decrease in blood pressure](https://image.slidesharecdn.com/01-150427073911-conversion-gate01/85/01-head-injuries-dr-phillip-bmc-81-320.jpg)
![History [cont’d]
Taken from an eye witness if the patient is unconscious or
from the patient
Include;-
Mechanism and full details of injury
For example:
Fall: Height, surface, posture of fall, point of contact
Motor vehicle collision: Speed, place in car, restraint, point of
impact
etc](https://image.slidesharecdn.com/01-150427073911-conversion-gate01/85/01-head-injuries-dr-phillip-bmc-83-320.jpg)
![History [cont’d]
Time of accident
Level of consciousness / unconscious?
Time of onset of unconsciousness
Duration of unconsciousness
Lucid interval
Amnesia [loss of memory]–
Retrograde Traumatic Amnesia
Post-traumatic amnesia](https://image.slidesharecdn.com/01-150427073911-conversion-gate01/85/01-head-injuries-dr-phillip-bmc-84-320.jpg)
![History [cont’d]
Current symptoms
Headache, vomiting, bleeding from ENT, LOC, fits, other associated
injuries
Pre-morbid illness
Diabetes mellitus
Renal diseases
Hypertension
Previous history of fits
History of medications and Allergies
Habit of taking alcohol or opium](https://image.slidesharecdn.com/01-150427073911-conversion-gate01/85/01-head-injuries-dr-phillip-bmc-85-320.jpg)
![Physical Examination
[cont’d]
Neck
Neck rigidity
Immobilization is required until stability is assured
Trunk
Evidence of chest injuries
Evidence of abdominal injuries
MSS [limbs, pelvis and spines]
Closed or open wounds, fractures
Neurological
Level of consciousness (GCS), pupilary size and reaction to light
Focal signs, brainstem reflexes, motor function](https://image.slidesharecdn.com/01-150427073911-conversion-gate01/85/01-head-injuries-dr-phillip-bmc-87-320.jpg)
![Imaging investigations
Skull x-rays
CT Scan brain/skull
MRI [Magnetic Resonance Imaging]
Cervical x-rays](https://image.slidesharecdn.com/01-150427073911-conversion-gate01/85/01-head-injuries-dr-phillip-bmc-90-320.jpg)
![CT Scan brain/skull
Investigation of choice
Can reveal
Bony injury
Haematomas
Evidence of cerebral edema
Mass effect [midline shift]
It is necessary for operative planning](https://image.slidesharecdn.com/01-150427073911-conversion-gate01/85/01-head-injuries-dr-phillip-bmc-92-320.jpg)
![CT Scan brain/skull [cont’d]
Indications
Moderate to severe head injury
Deteriorating levels of consciousness
Depressed fractures
Focal neurological deficits
Evidence of basilar fracture
Penetrating head trauma
Persistent severe headache and vomiting
Seizures](https://image.slidesharecdn.com/01-150427073911-conversion-gate01/85/01-head-injuries-dr-phillip-bmc-93-320.jpg)
![Magnetic Resonance Imaging
[MRI]
Has no role in acute management of patients with head injury
Can be used in case of diffuse axonal injury and in follow-up
prognostication
Able to detect small lesions in vital areas of brain not seen by
CT scan
Preserved for later detail evaluation after acute problem has
been addressed](https://image.slidesharecdn.com/01-150427073911-conversion-gate01/85/01-head-injuries-dr-phillip-bmc-94-320.jpg)
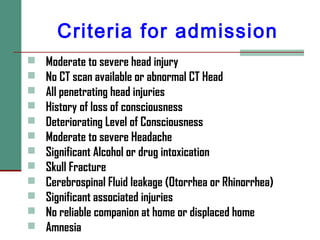
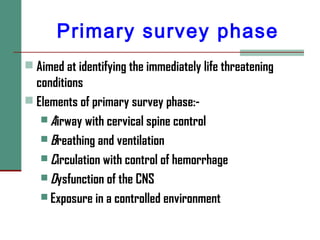
![MANAGEMENT
Criteria for admission
The management of head injury follow Advanced Trauma
Life Support [ATLS] guideline
6 phases
Primary survey phase
Resuscitation phase
Secondary survey phase
Tertiary survey phase
Supportive care phase
Definitive care phase](https://image.slidesharecdn.com/01-150427073911-conversion-gate01/85/01-head-injuries-dr-phillip-bmc-100-320.jpg)
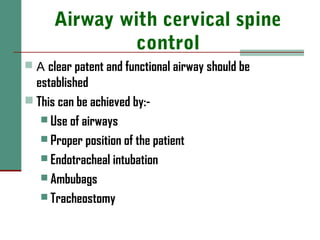
![Resuscitation phase
Done simultaneously with primary survey phase
Needs multidisciplinary approach
Aimed at treating the immediately life threatening
conditions
Establish a patent airway and immobilization of cervical
spine
Ensure breathing and adequate ventilatory support
Restore circulatory volume and h’ge control
Brief neurological evaluation
Fully expose [undress] the patient](https://image.slidesharecdn.com/01-150427073911-conversion-gate01/85/01-head-injuries-dr-phillip-bmc-103-320.jpg)
![Supportive care phase
Position:
In a recovery position
Elevate the head by 15-30
o
[take care of cervical fracture]
2 hourly turning to avoid pressure sores
Urethral catheterization to empty the bladder in order to:-
Avoid renal complications
Enable good record of his output to be kept
To ensure the bed is dry
NGT should be inserted in all patients with severe head injury
except patient with nasal bleeding and rhinorrhoea
To empty the stomach and for feeding](https://image.slidesharecdn.com/01-150427073911-conversion-gate01/85/01-head-injuries-dr-phillip-bmc-111-320.jpg)
![Supportive care phase
[cont’d]
Monitor:
Levels of consciousness
Pupillary size and reaction to light
Vital signs
Input-output chart
Motor and sensory functions
Nutrition support
Patients who started on nutrition earlier have better out
come than when it is started later](https://image.slidesharecdn.com/01-150427073911-conversion-gate01/85/01-head-injuries-dr-phillip-bmc-112-320.jpg)

![Osmotherapy
Intended to draw water out of the brain by an osmotic
gradient and to decrease blood viscosity
These changes decrease ICP and increase CBF
Include
Mannitol
Diuretics [loop] –e.g. Frusemide](https://image.slidesharecdn.com/01-150427073911-conversion-gate01/85/01-head-injuries-dr-phillip-bmc-118-320.jpg)
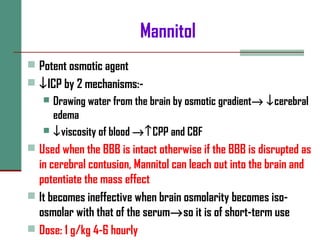
![Diuretics [loop]
E.g. Frusemide
Potent osmotic agent
Reduces ICP by reducing cerebral edema and CSF production
It may act synergistically with mannitol](https://image.slidesharecdn.com/01-150427073911-conversion-gate01/85/01-head-injuries-dr-phillip-bmc-120-320.jpg)