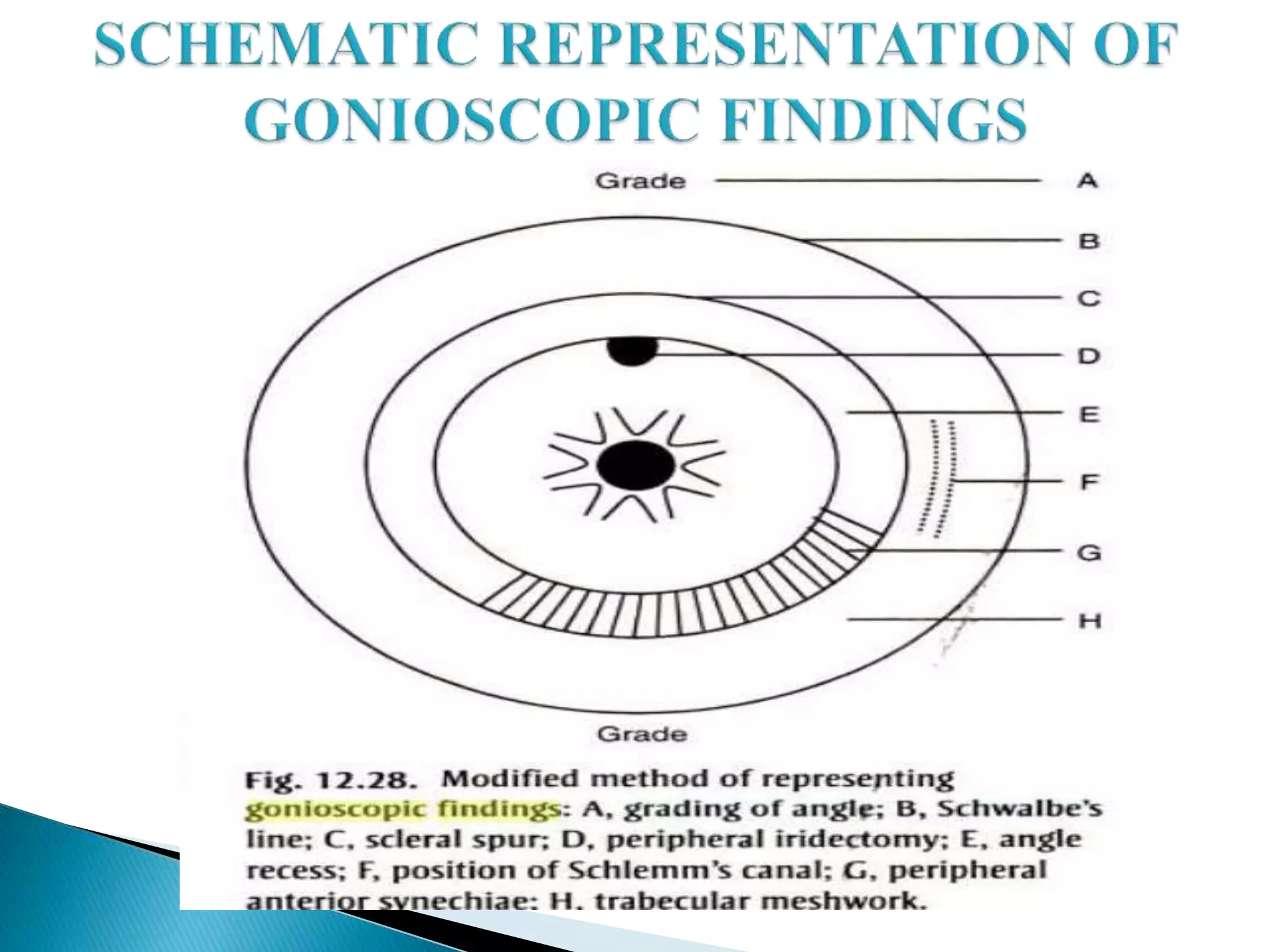
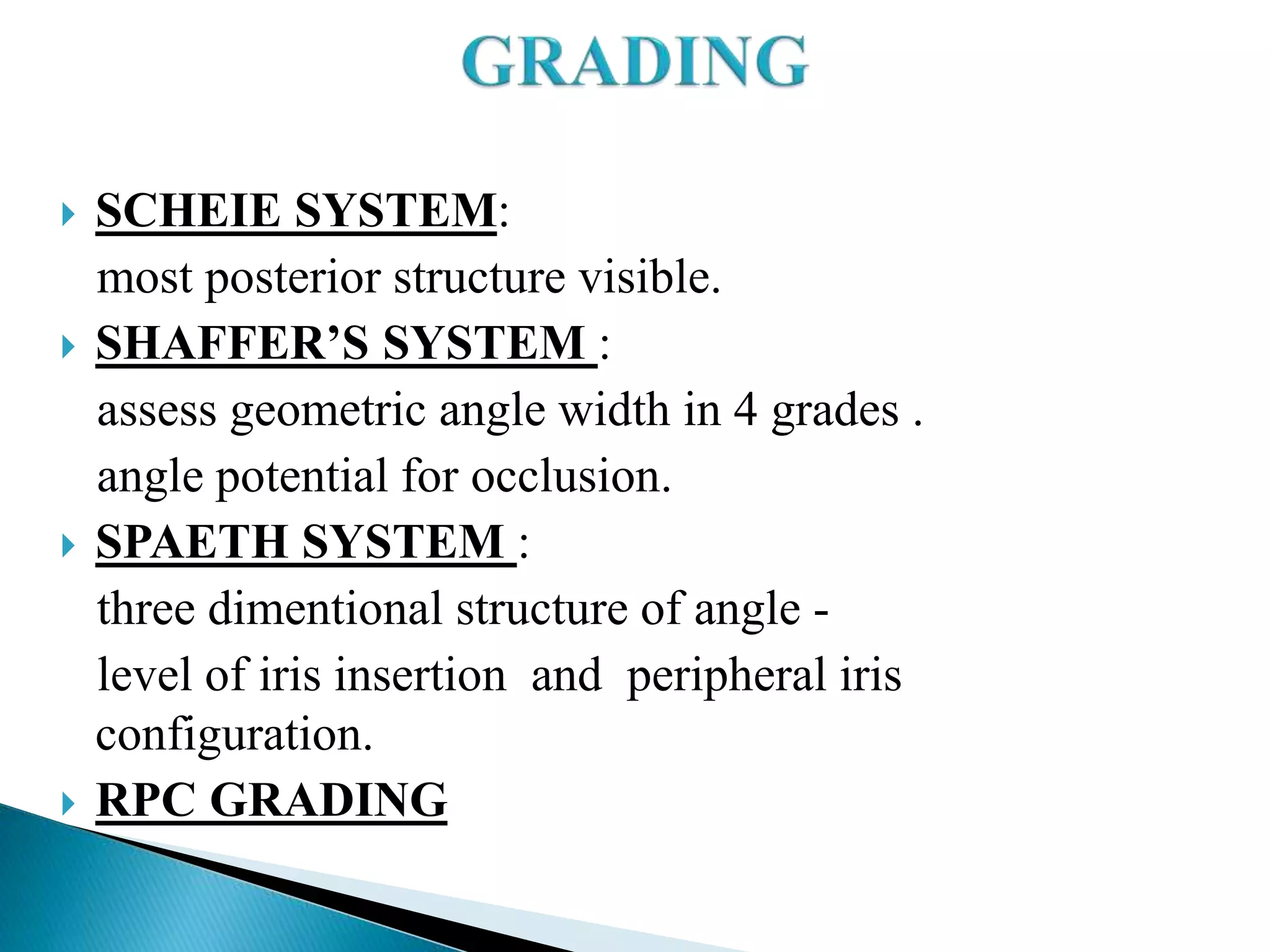
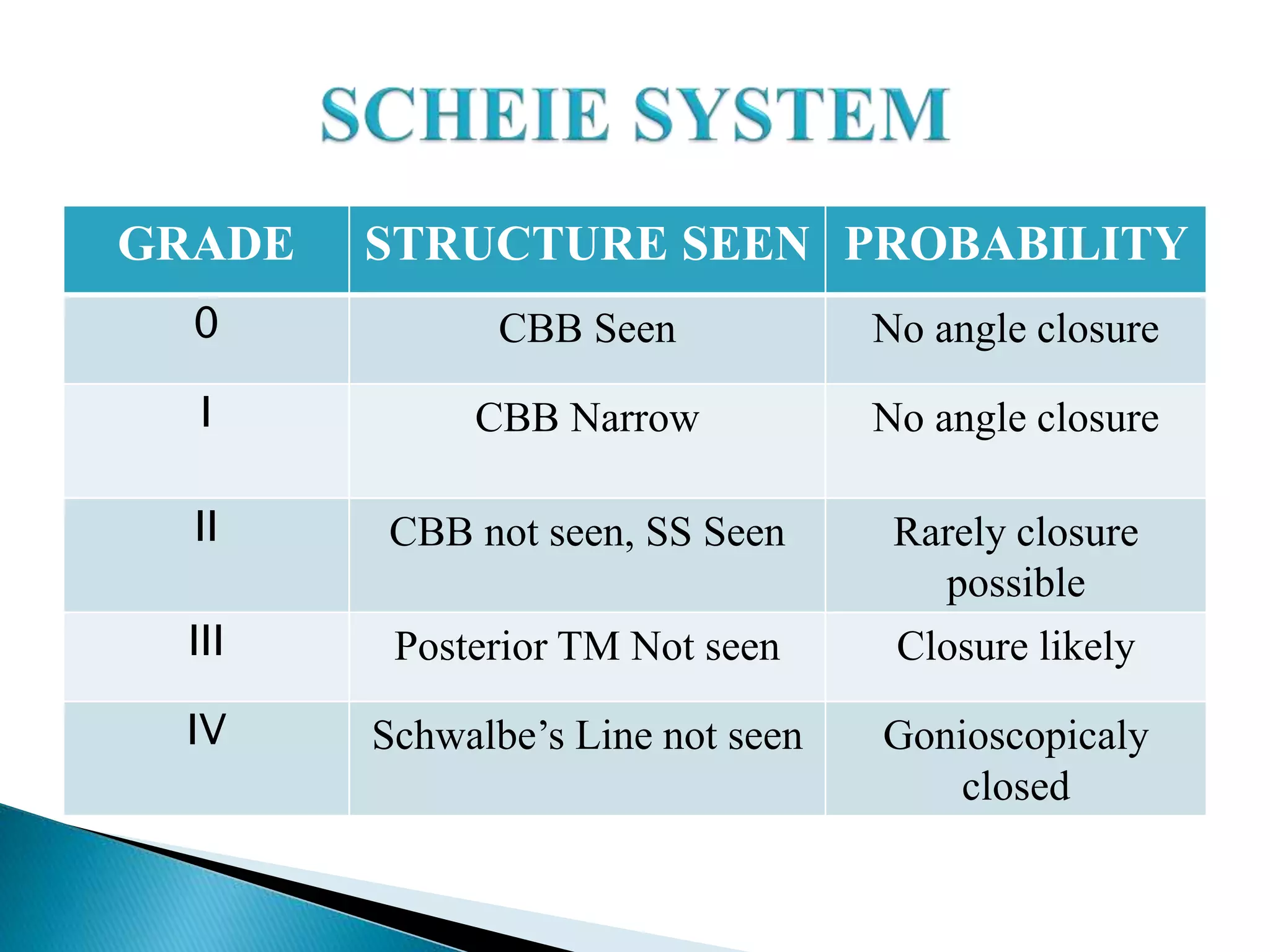
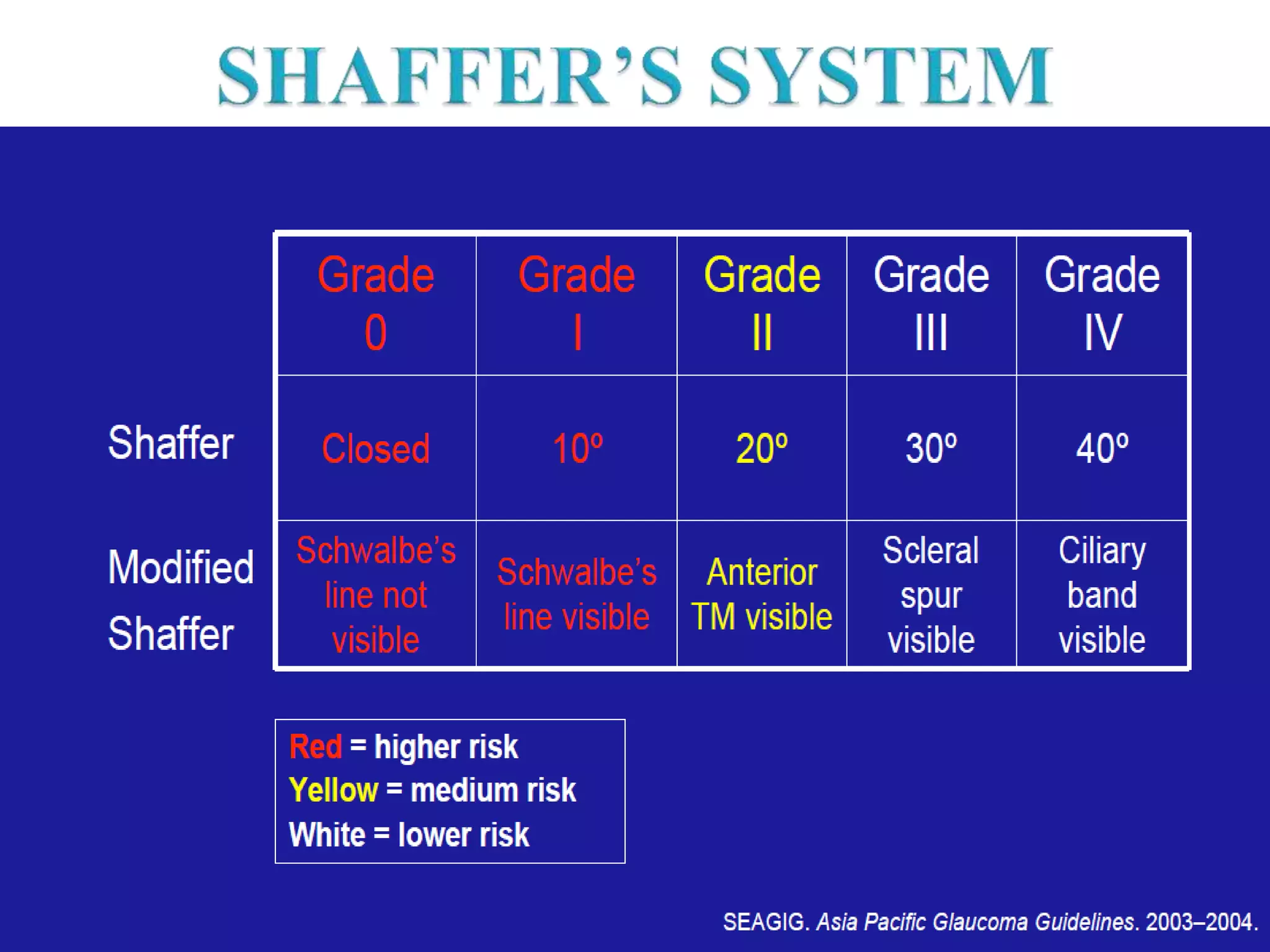
The document discusses the history and development of gonioscopy. It notes that gonioscopy was first visualized by Alexois Trantas in 1907 and Maximilian Salsmann in 1914 is considered the father of gonioscopy. It describes improvements to contact lenses and development of gonioprisms by Koeppe, Uribe Troncoso, Barkan, and Goldmann. The document provides details on various gonioscopy lenses and their uses. It discusses the advantages and disadvantages of direct vs indirect gonioscopy and classifications used to grade the iridocorneal angle.
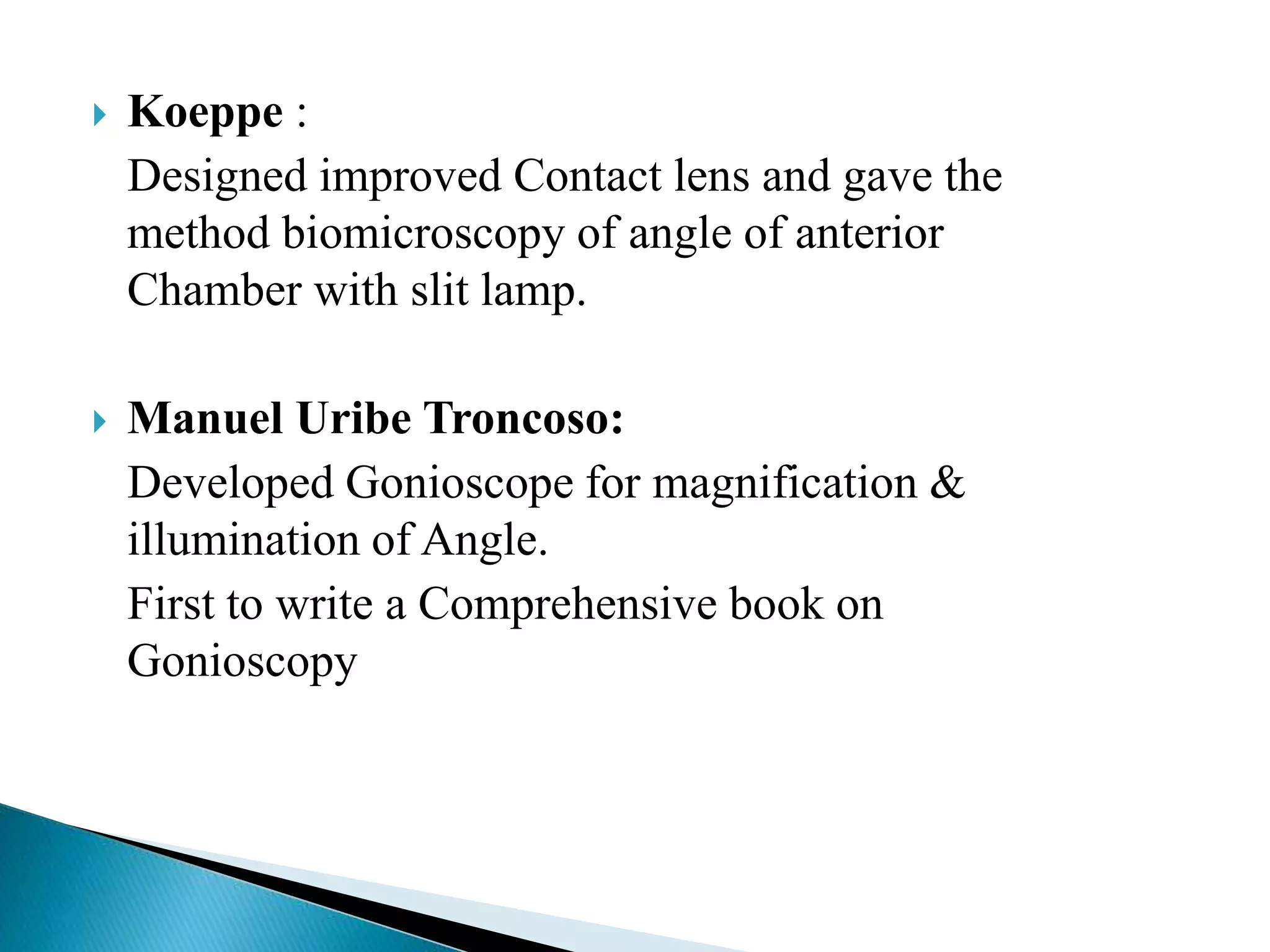
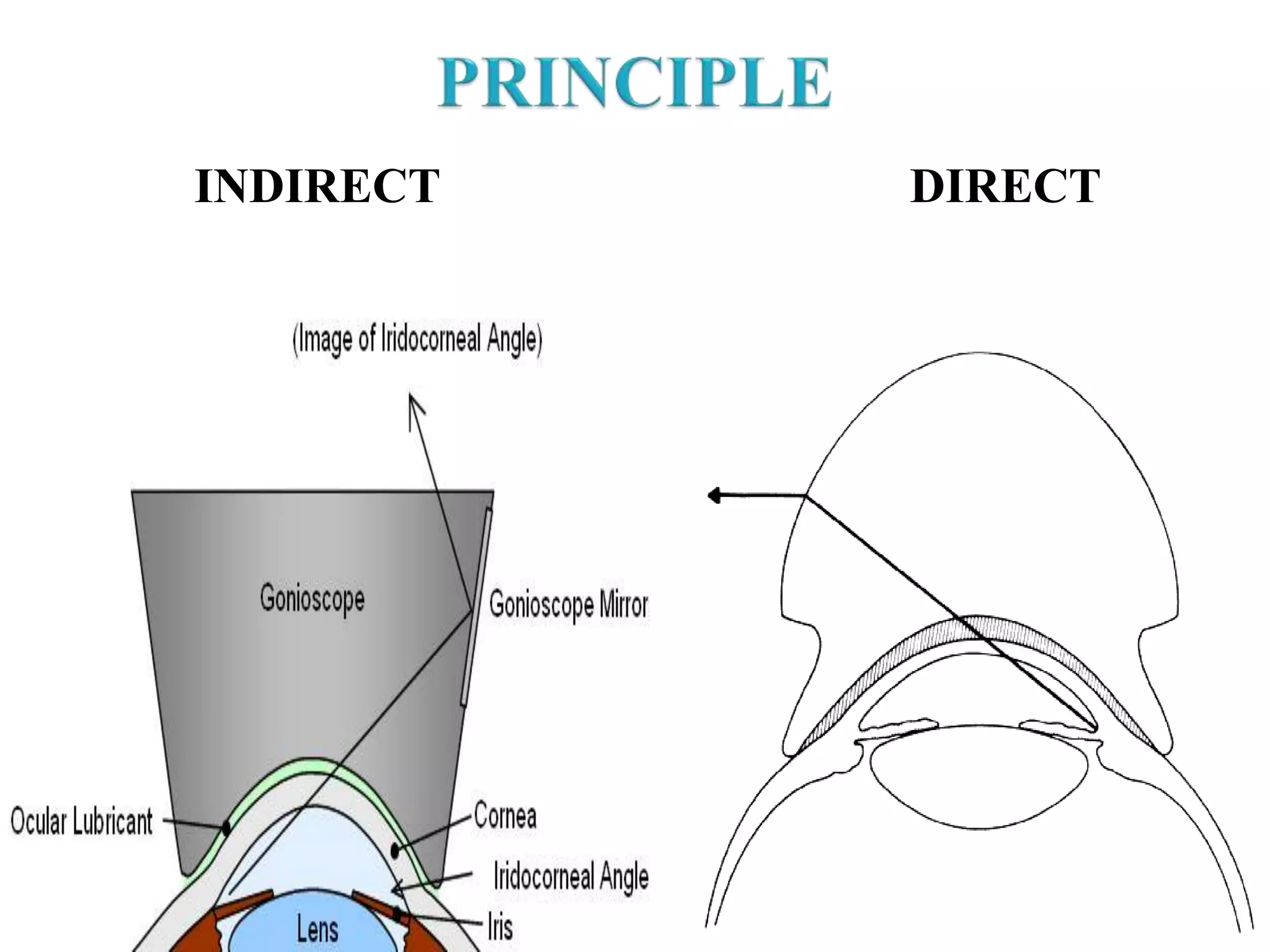




![DIRECT INDIRECT
Panoramic view of
iridocorneal angle with
ability to adjust view by
examiner.
Both eyes can be examined
simultaneously.
No viscous [ coupling ]
material required.
Direct view for surgery e.g.
Goniotomy
DISADV: Inability to
perform indentation, low
magnification, assistance.
Segmental View
One Eye at a time
Viscous required
Mirror Image seen
Excellent optics with Slit
Lamp
Indentation Can be Done](https://image.slidesharecdn.com/gonioscopy-140723150732-phpapp01/75/Gonioscopy-25-2048.jpg)

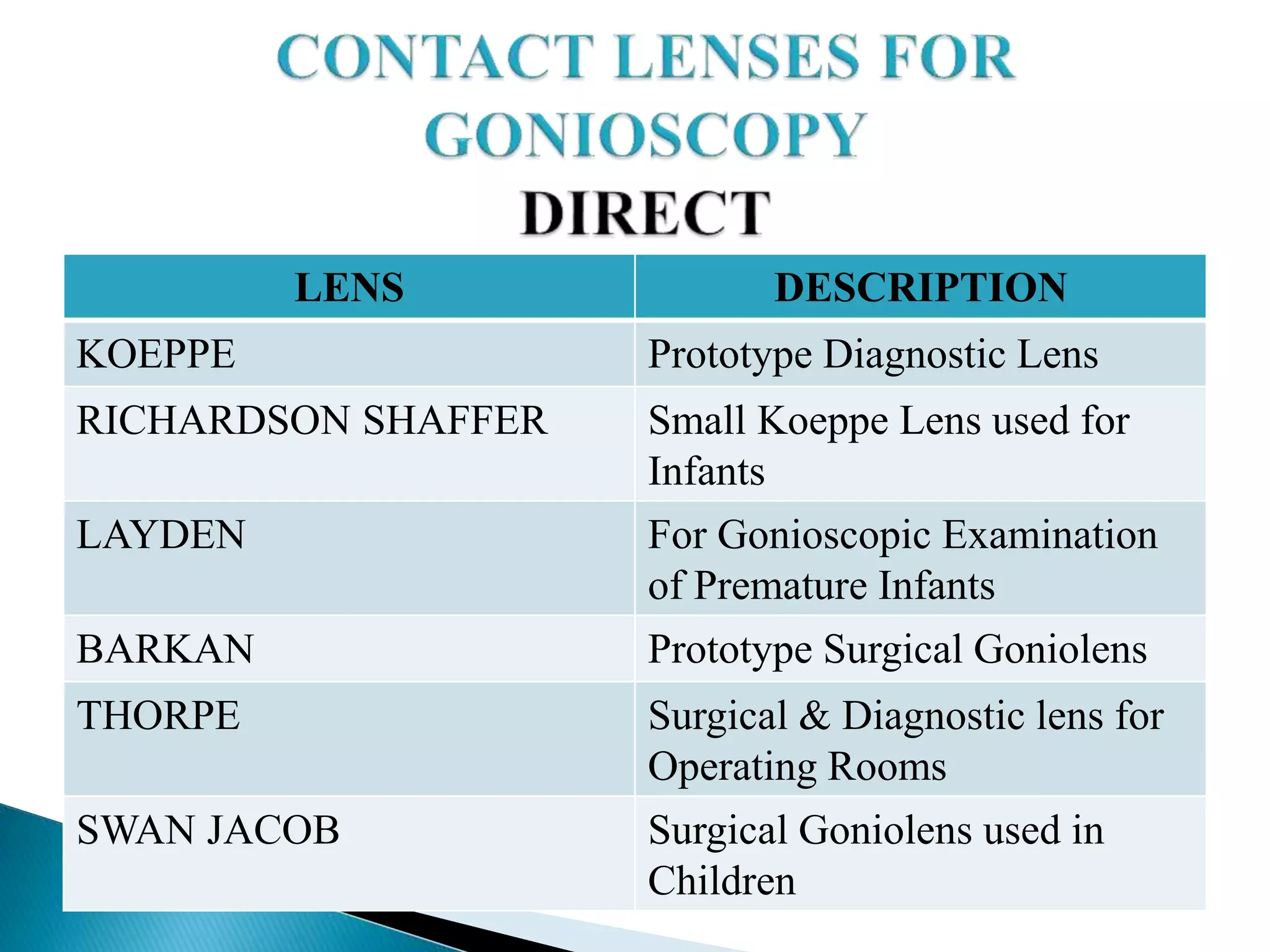
![ If posterior [ pigmented ] part of trabecular
meshwork is not visible in more than 180
degrees of angle without indentation or
manipulation, this is known as an ‘ occludable
angle’.](https://image.slidesharecdn.com/gonioscopy-140723150732-phpapp01/75/Gonioscopy-54-2048.jpg)


![ Wash with soap & water
Soaking the lens for 5-10 min in fresh solution of Sod.
Hypochlorite [ 1:10 household bleach : water]
Rinsing with sterile water
Air drying
3% H2O2 or 1% Formaldehyde can also be used.
Direct surgical gonioscopes [ Koeppe, Swan Jacob] can
be sterilized with ethylene oxide.](https://image.slidesharecdn.com/gonioscopy-140723150732-phpapp01/75/Gonioscopy-83-2048.jpg)