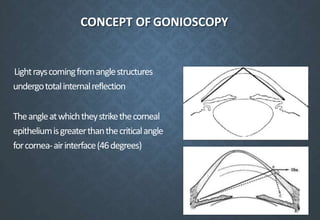
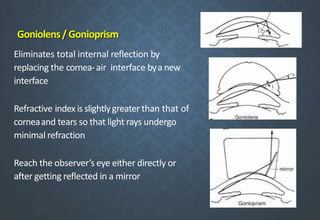
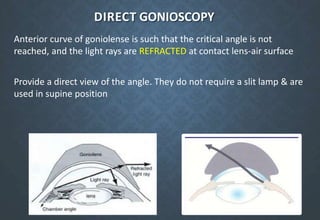
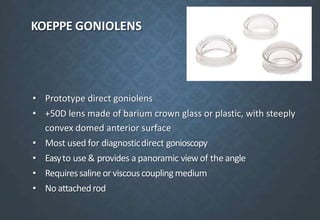
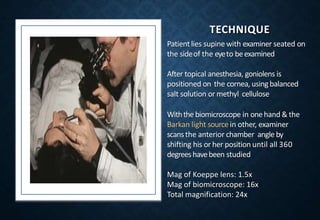
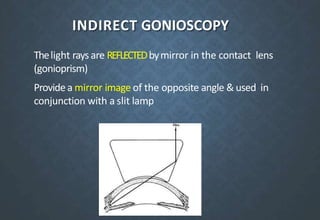
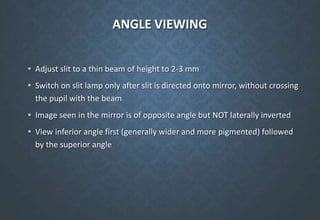
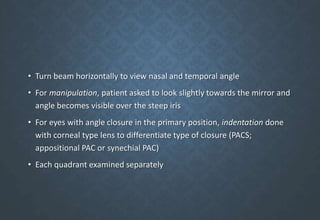
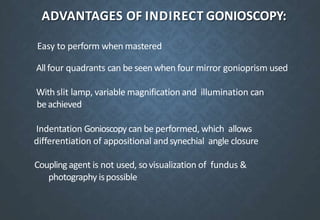
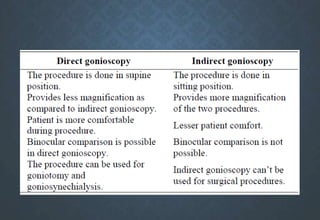
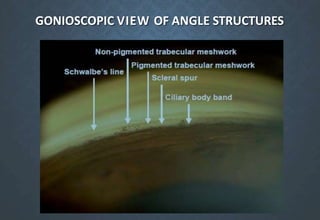
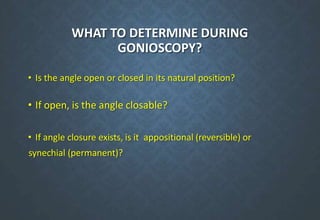
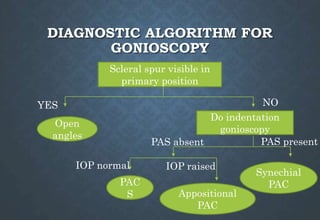
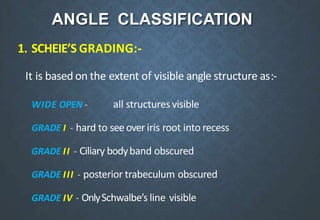
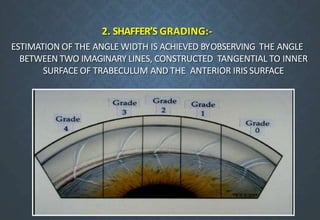
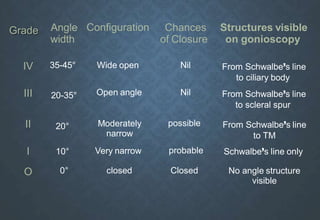
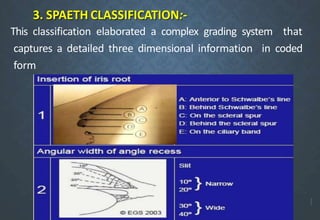
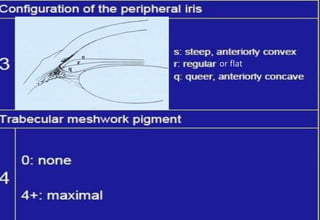
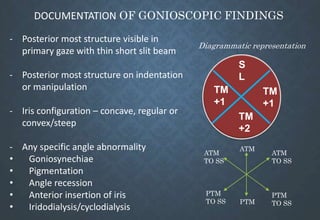
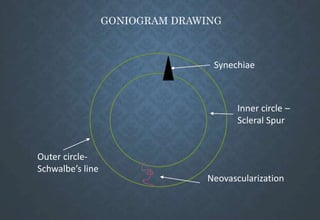
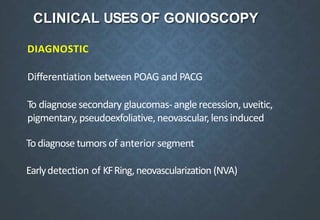
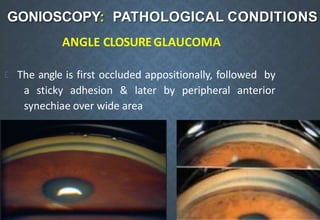
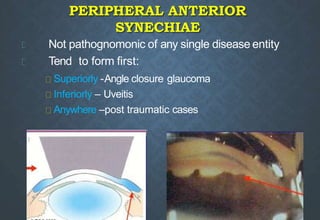
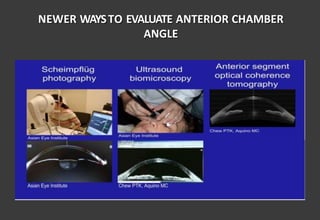
Gonioscopy allows examination of the anterior chamber angle using specialized lenses or prisms. It is used diagnostically to differentiate glaucoma types and prognostically to detect conditions that may cause future angle closure. There are two main methods: direct gonioscopy uses convex lenses to directly view the angle while indirect uses prisms and a slit lamp to provide an inverted mirrored image. Findings are documented using grading scales to classify angle width and structures visible. It is invaluable for glaucoma diagnosis and guiding treatment decisions.