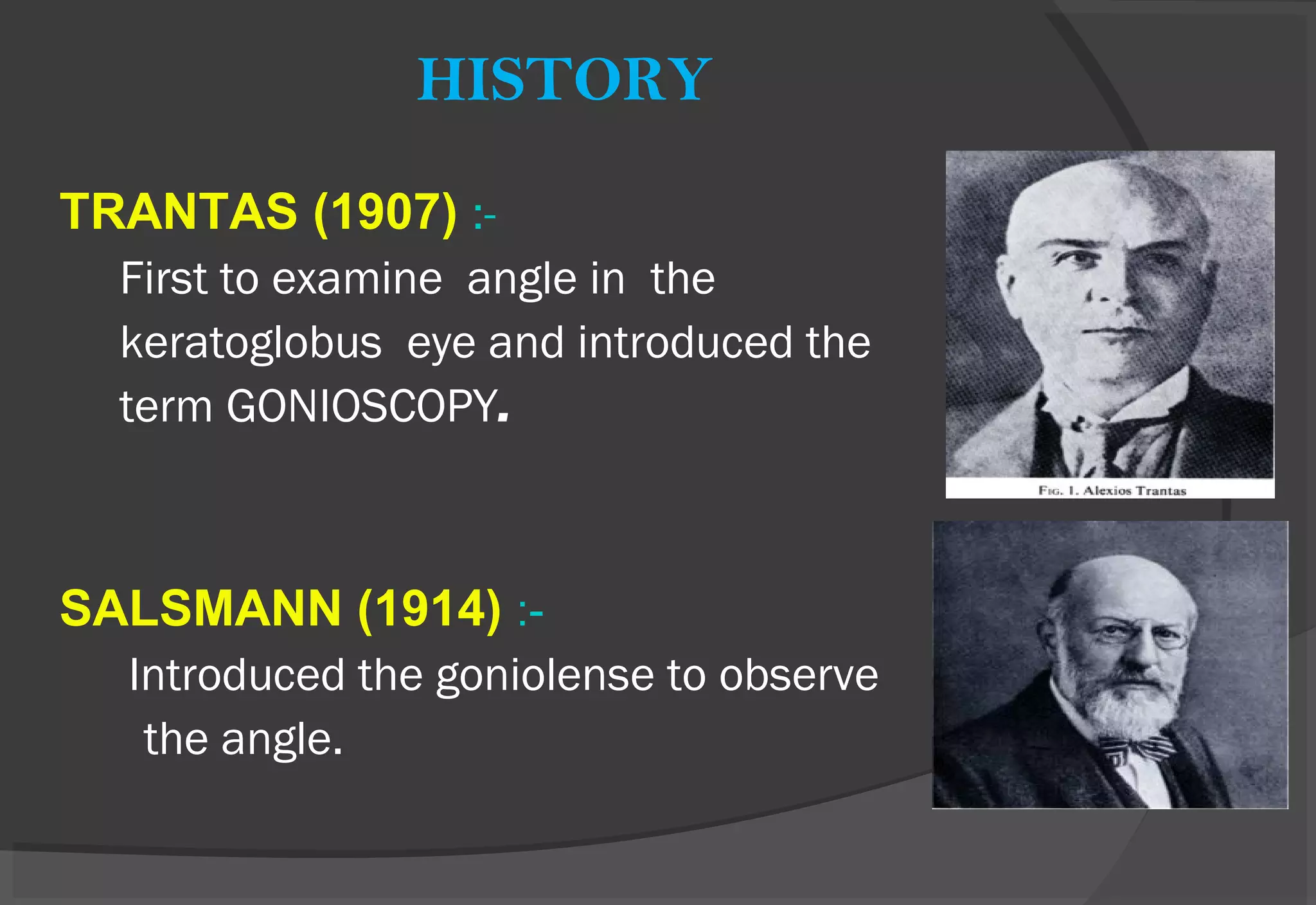
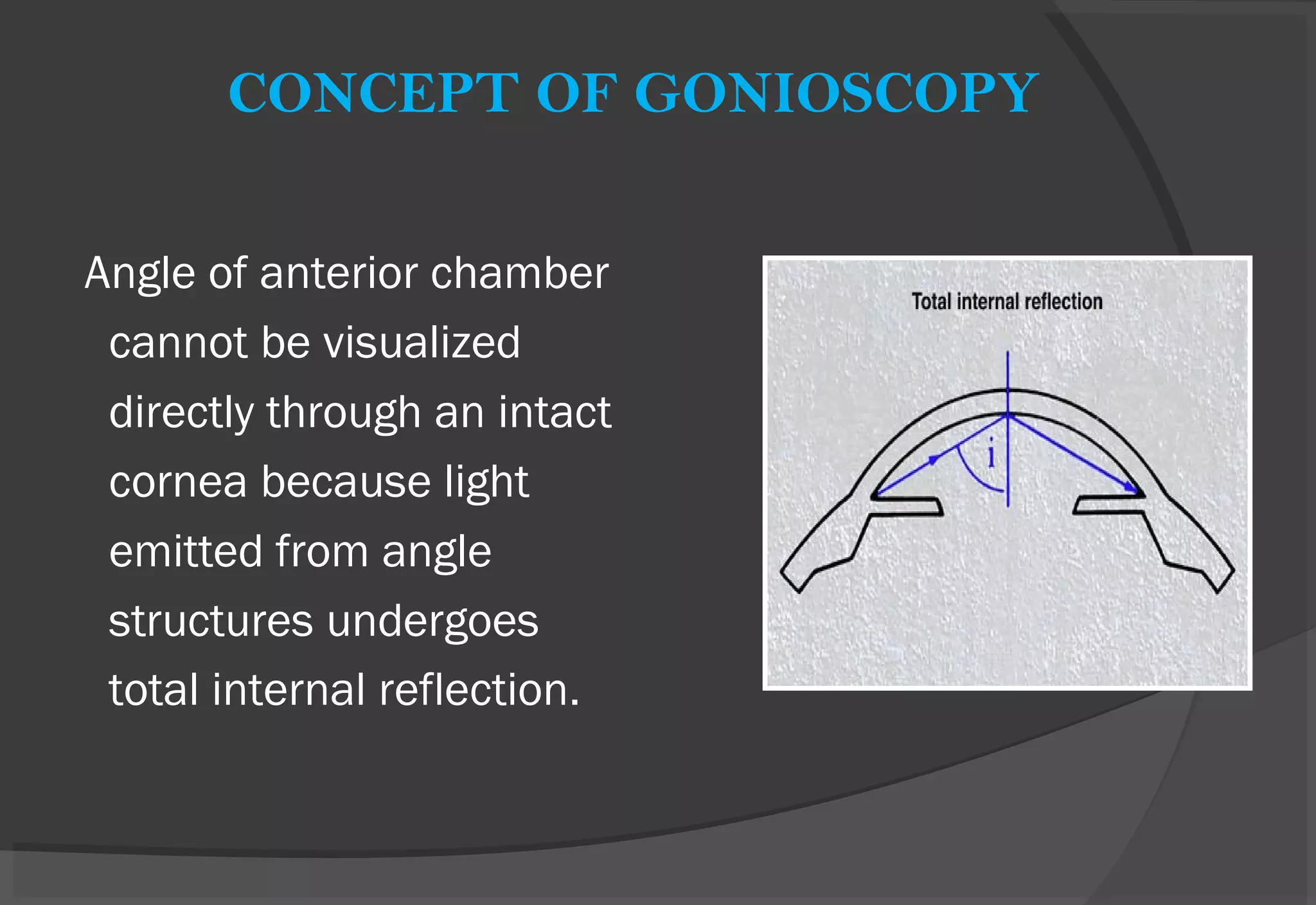
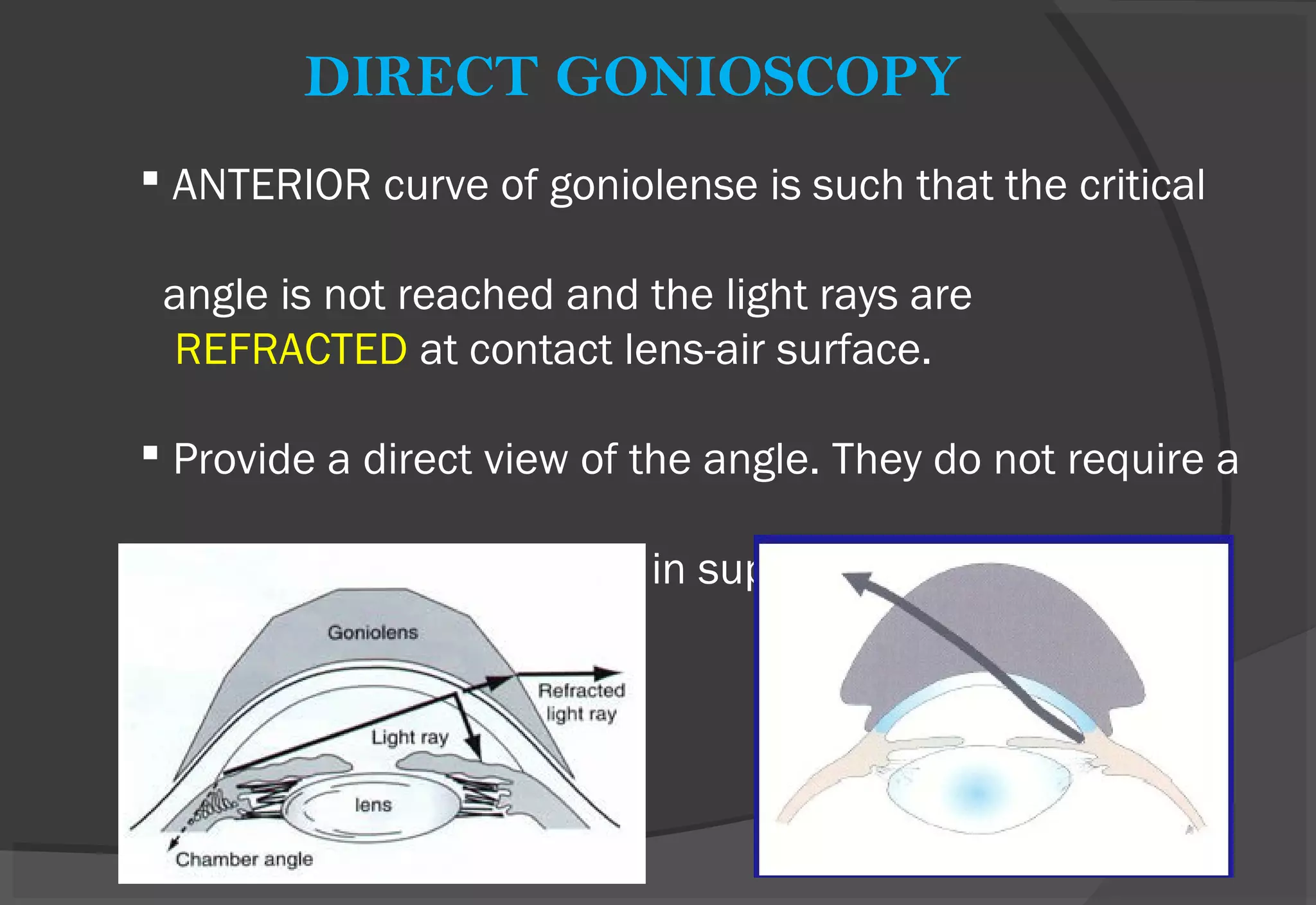
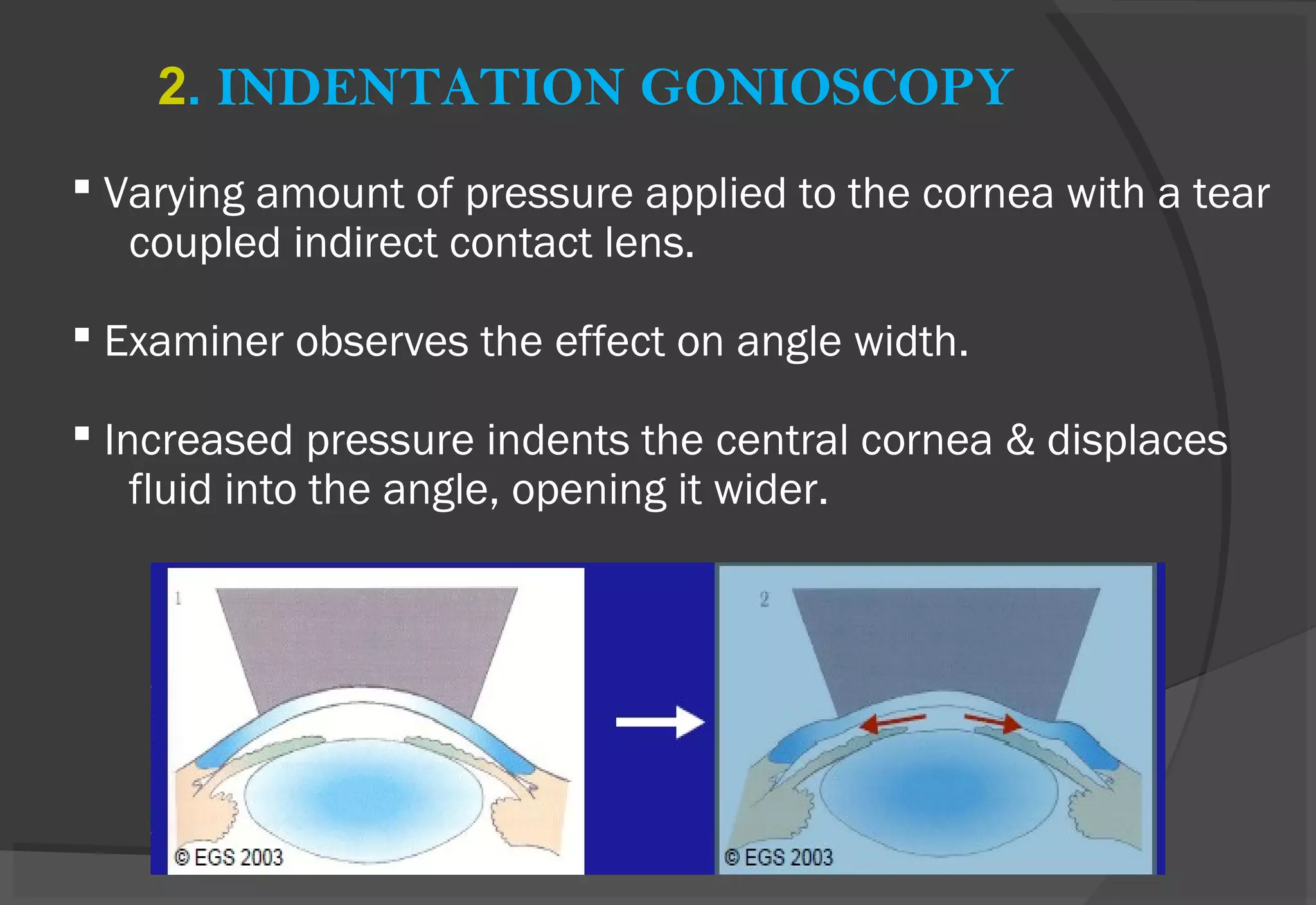
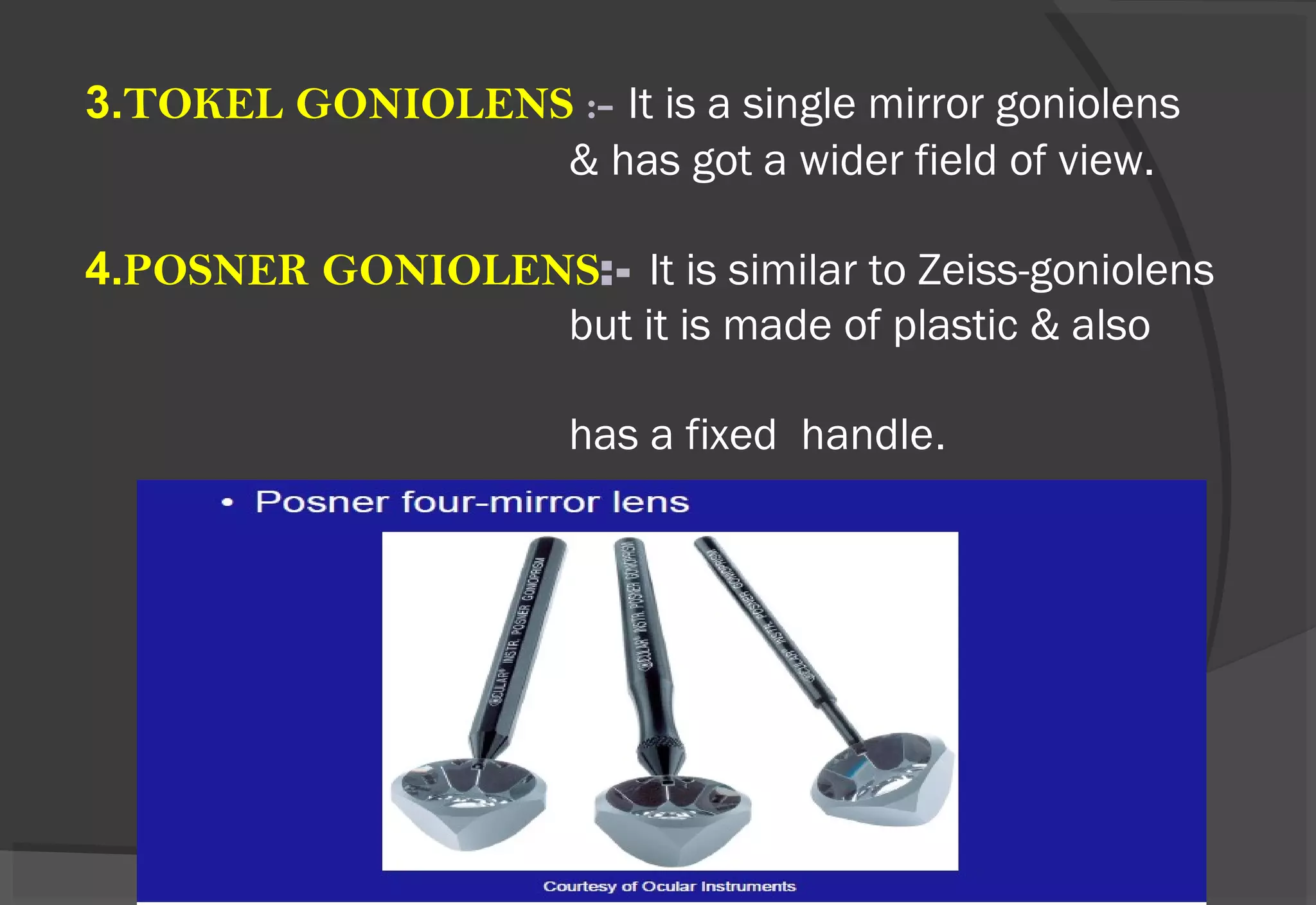
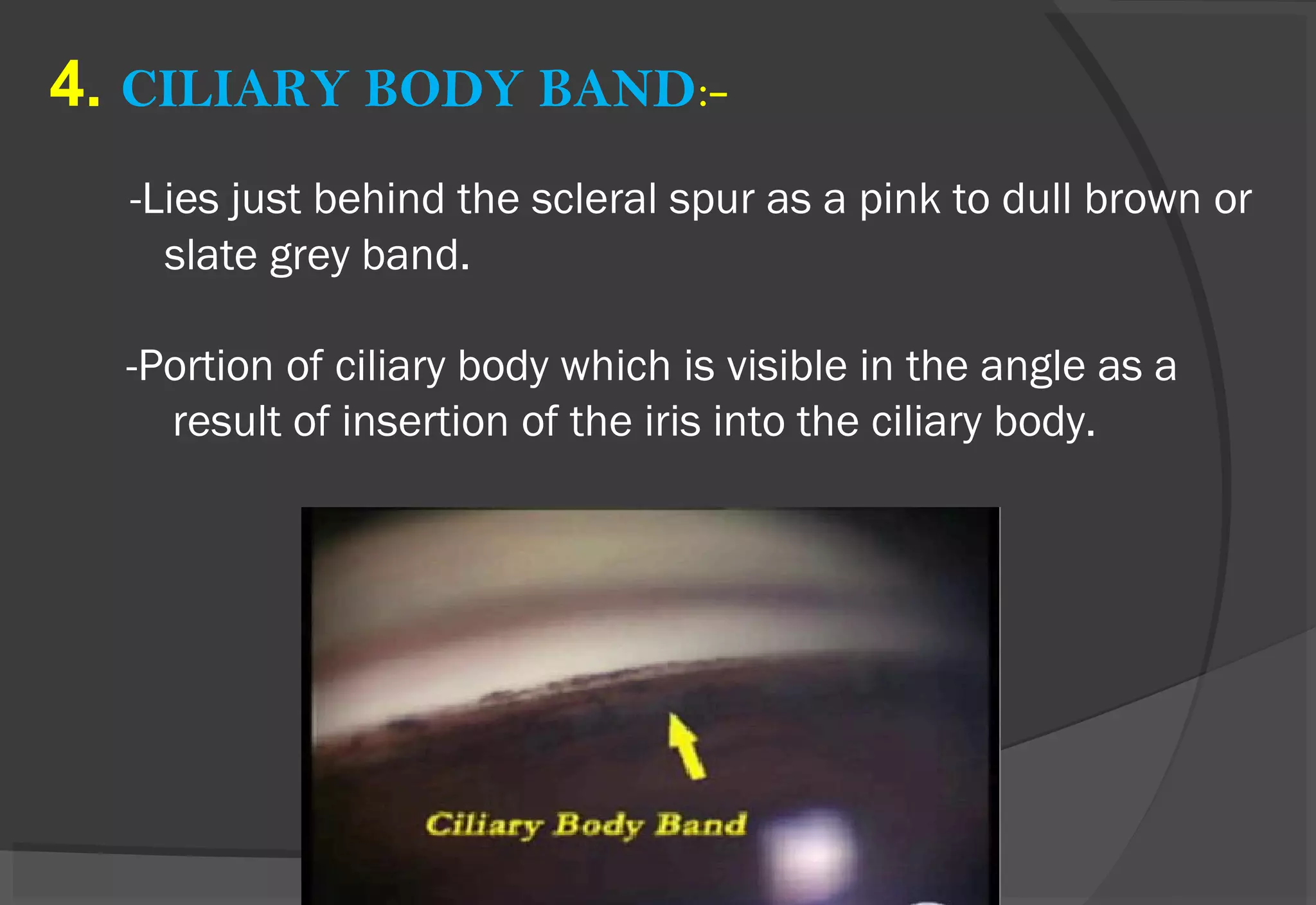
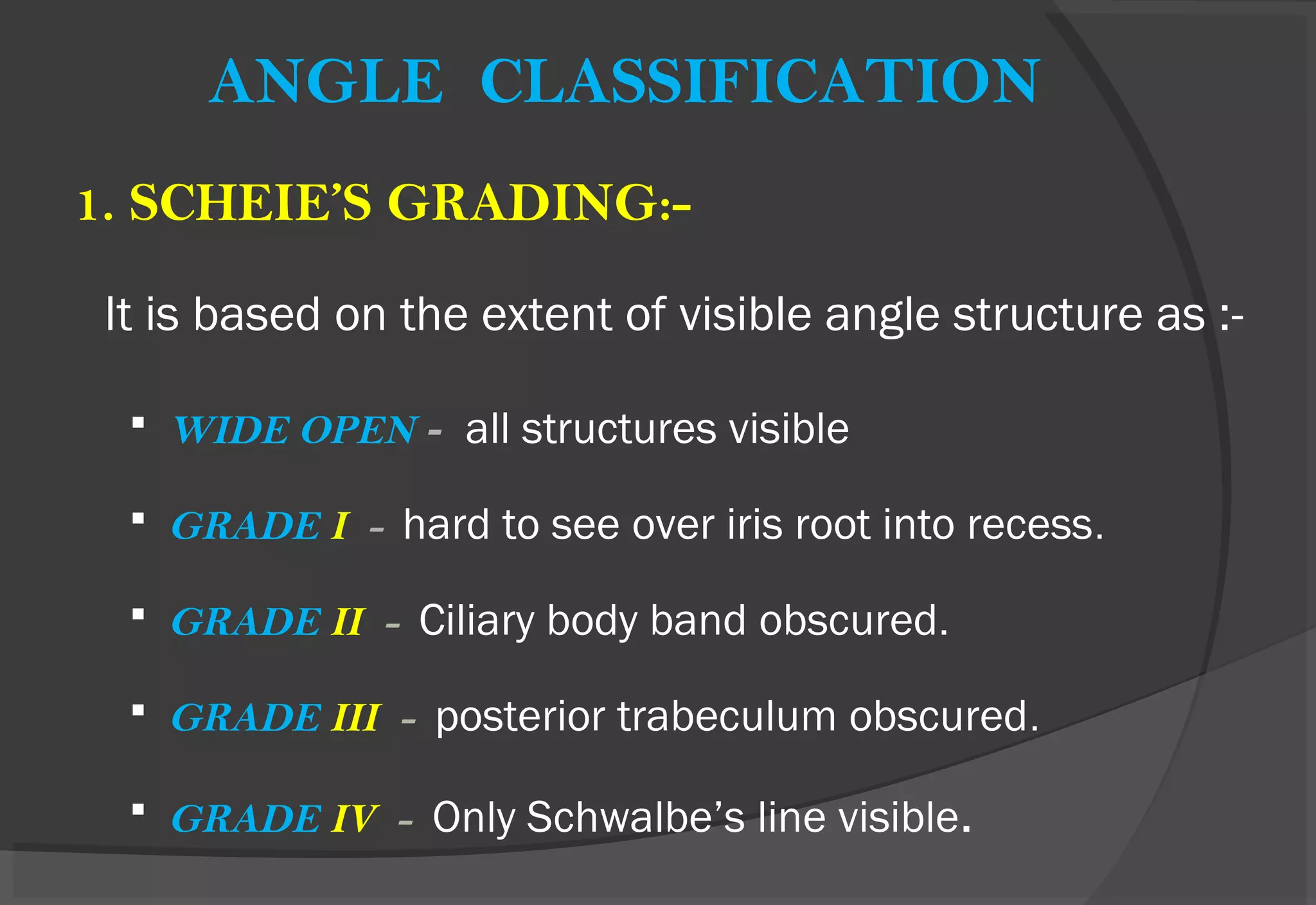
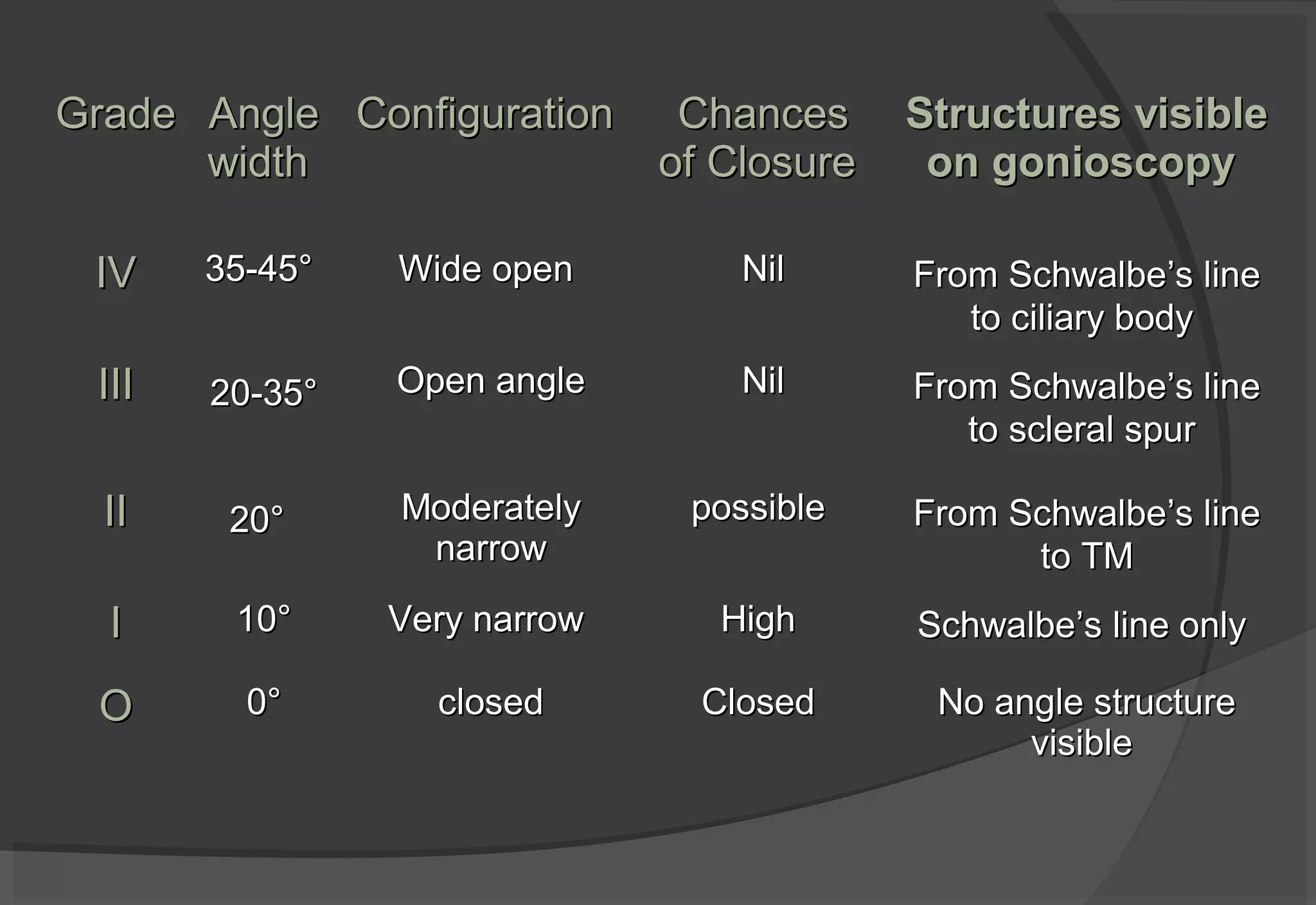
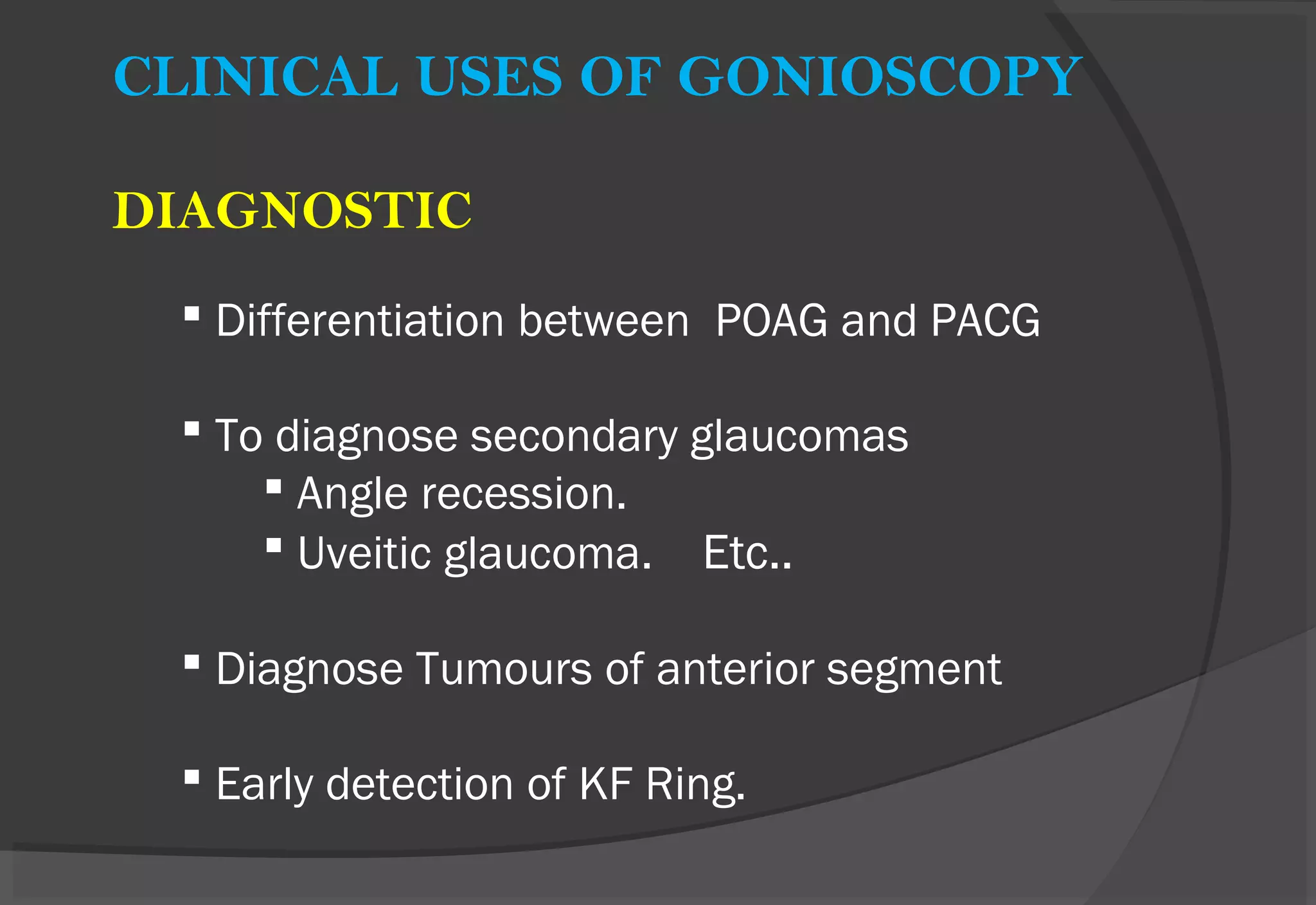
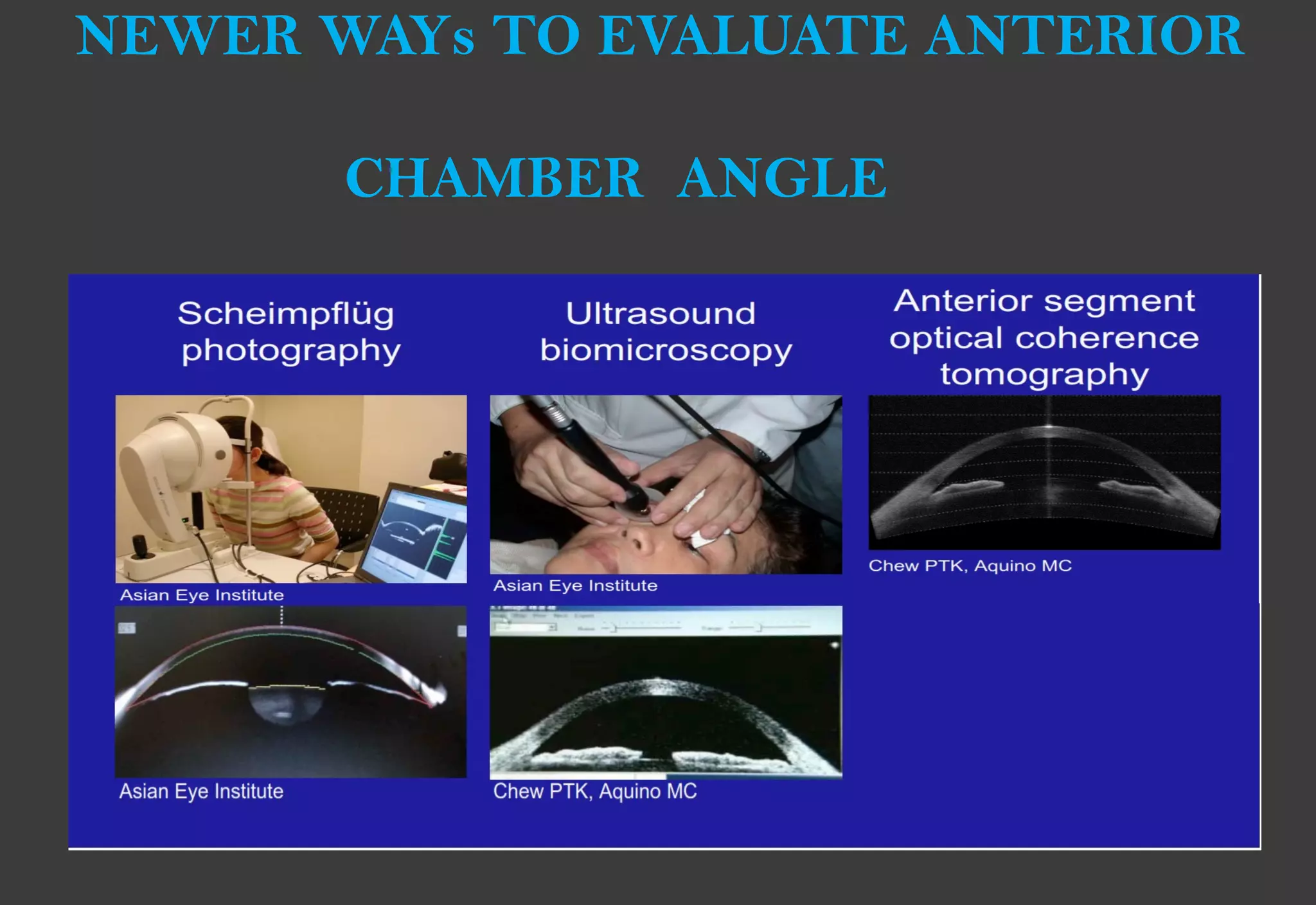
Gonioscopy allows visualization of the anterior chamber angle to evaluate for angle closure and diagnose glaucoma. It was pioneered in the early 20th century with the introduction of contact lenses to eliminate total internal reflection at the cornea. Direct gonioscopy uses contact lenses for a straight view, while indirect gonioscopy uses prisms for an inverted image at the slit lamp. Examination of angle structures like the trabecular meshwork and classification systems help diagnose angle closure and glaucoma. Gonioscopy is used for diagnostic and therapeutic purposes like laser and surgery.