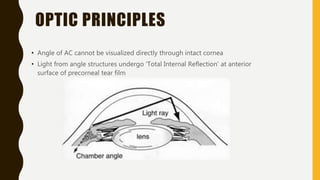
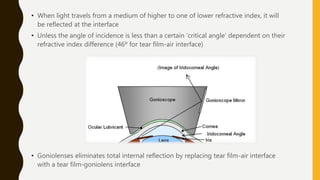
1. Gonioscopy is a technique used to evaluate the anterior chamber angle by using specialized contact lenses called goniolenses to eliminate total internal reflection and allow visualization of angle structures.
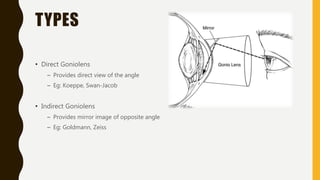
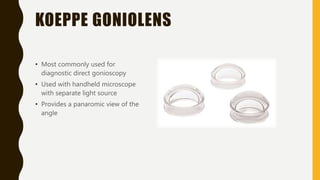
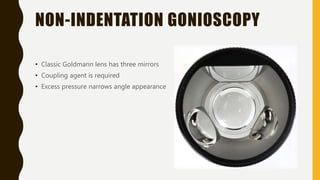
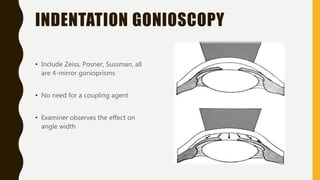
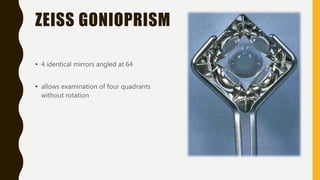
2. There are two main types of goniolenses - direct goniolenses that provide a direct view, and indirect goniolenses that provide a mirror image view using prisms.
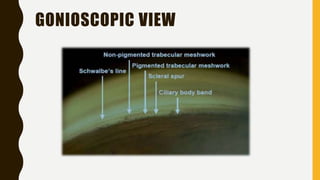
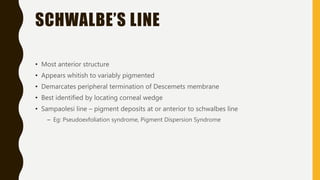
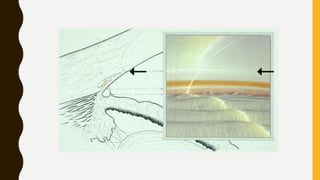
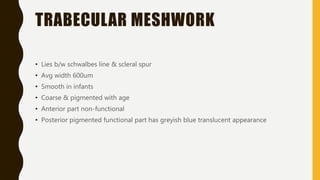
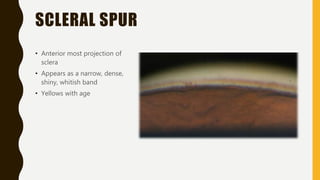
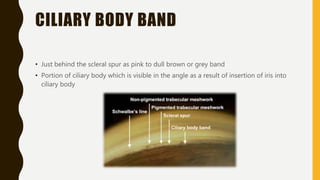
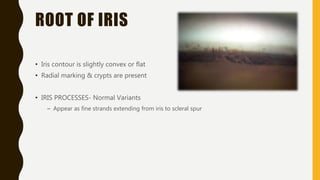
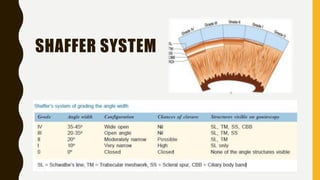
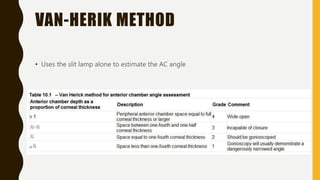
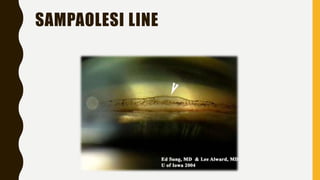
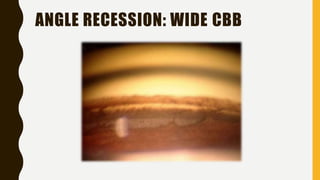
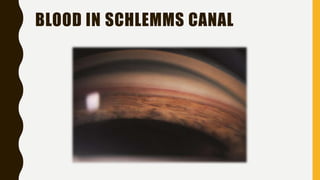
3. Important structures visible on gonioscopy include Schwalbe's line, the trabecular meshwork, scleral spur, ciliary body band, and root of iris. Angle width can be graded using systems like Shaffer or Van Herick.