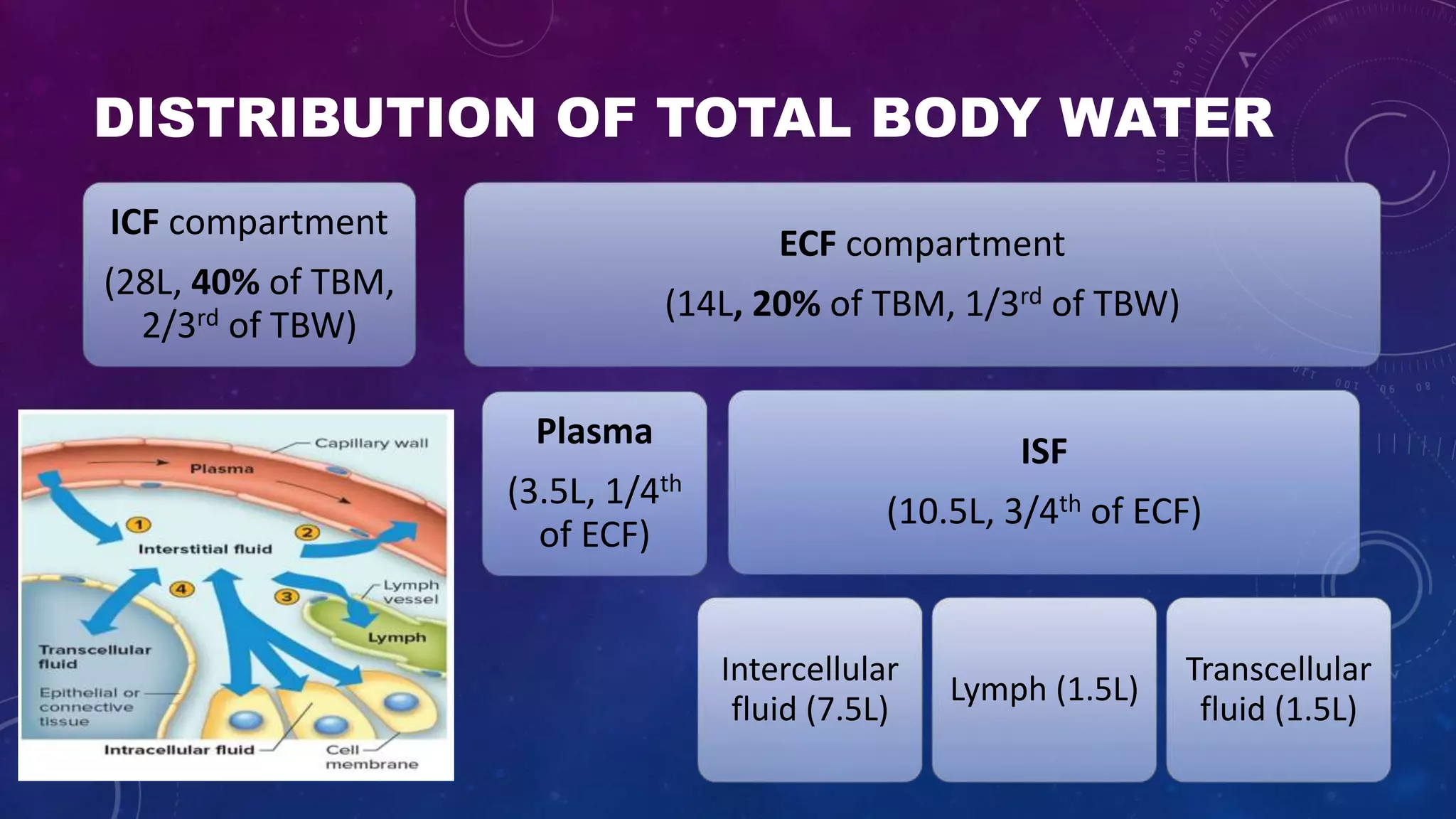
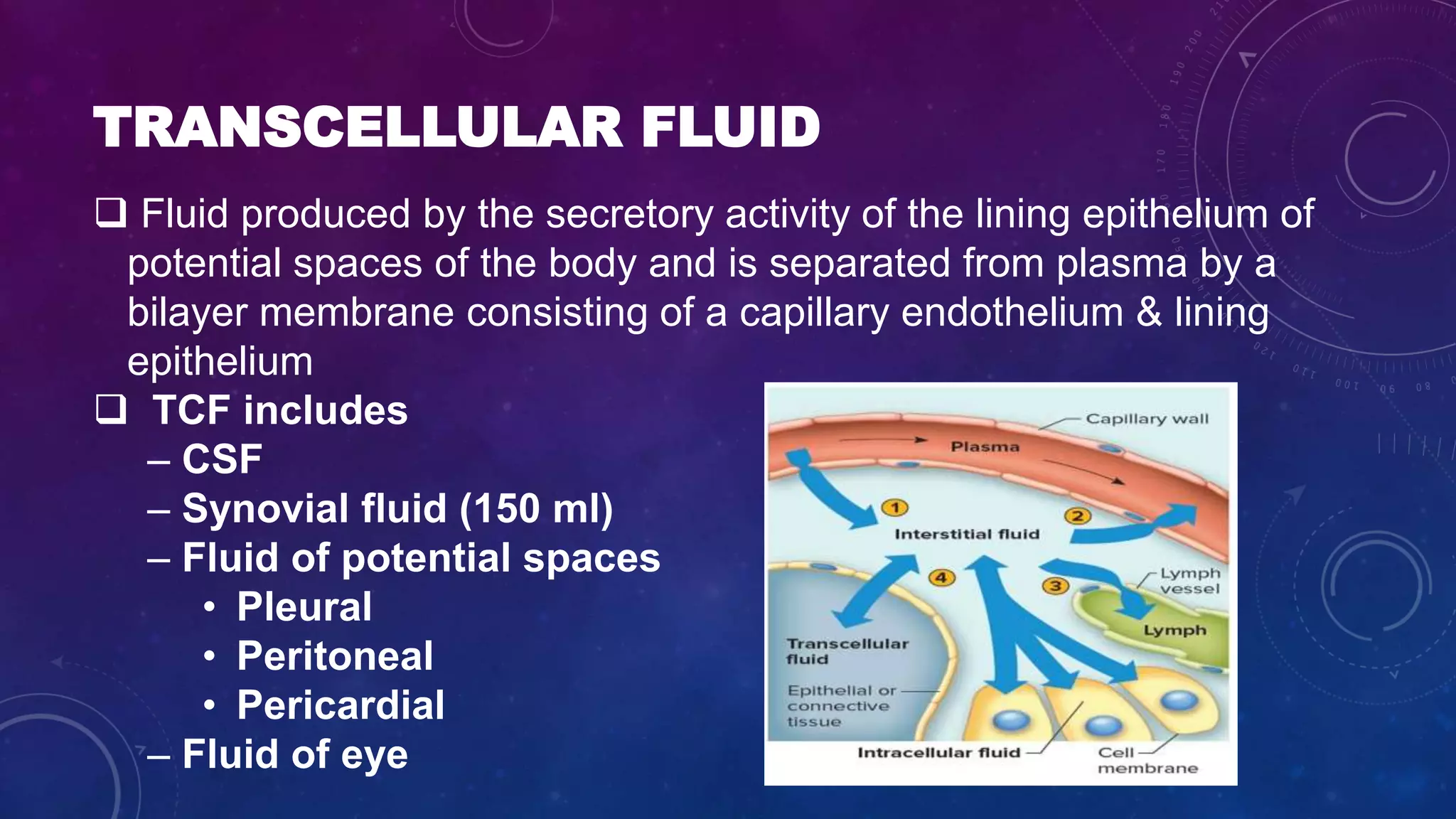
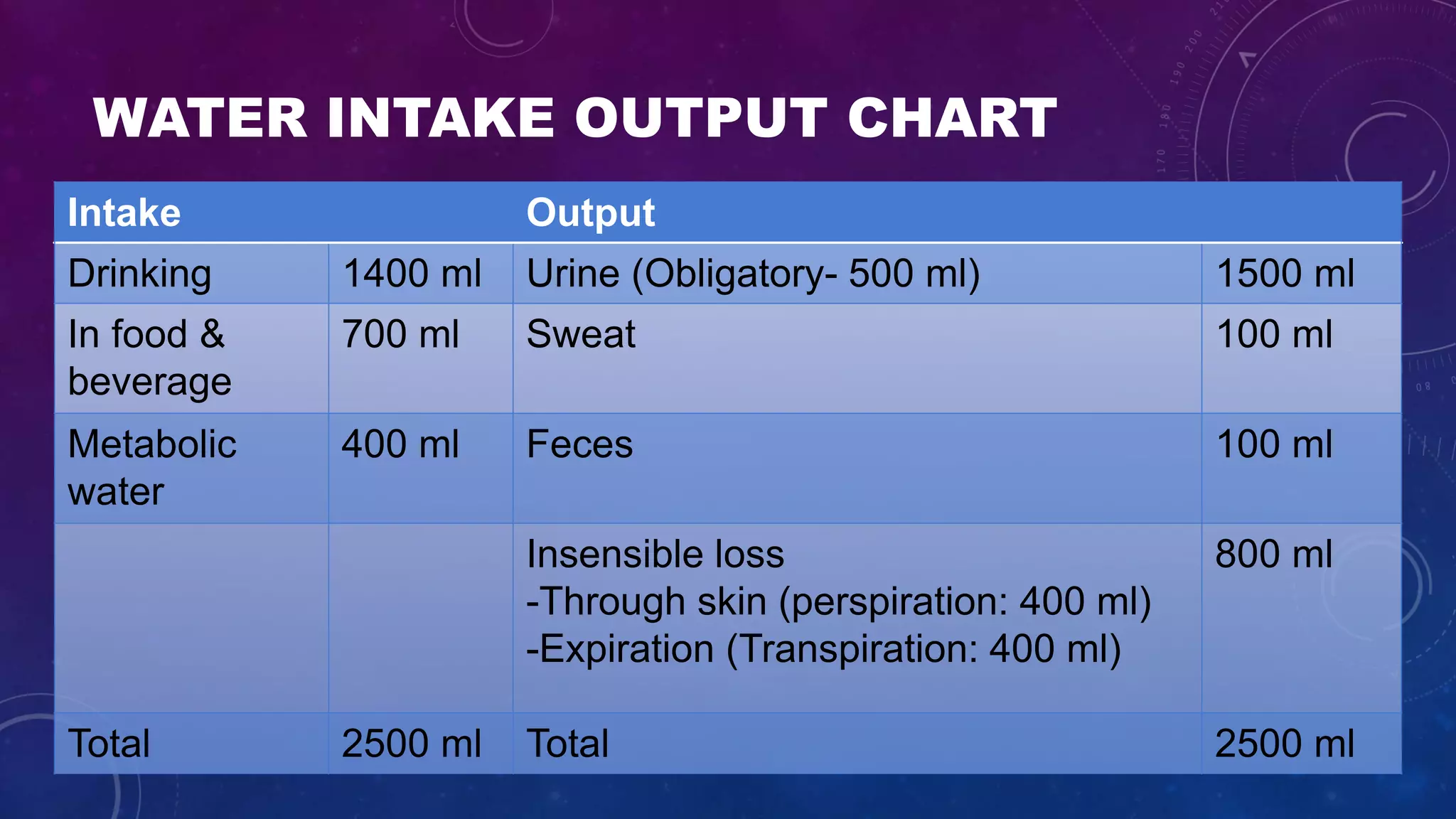
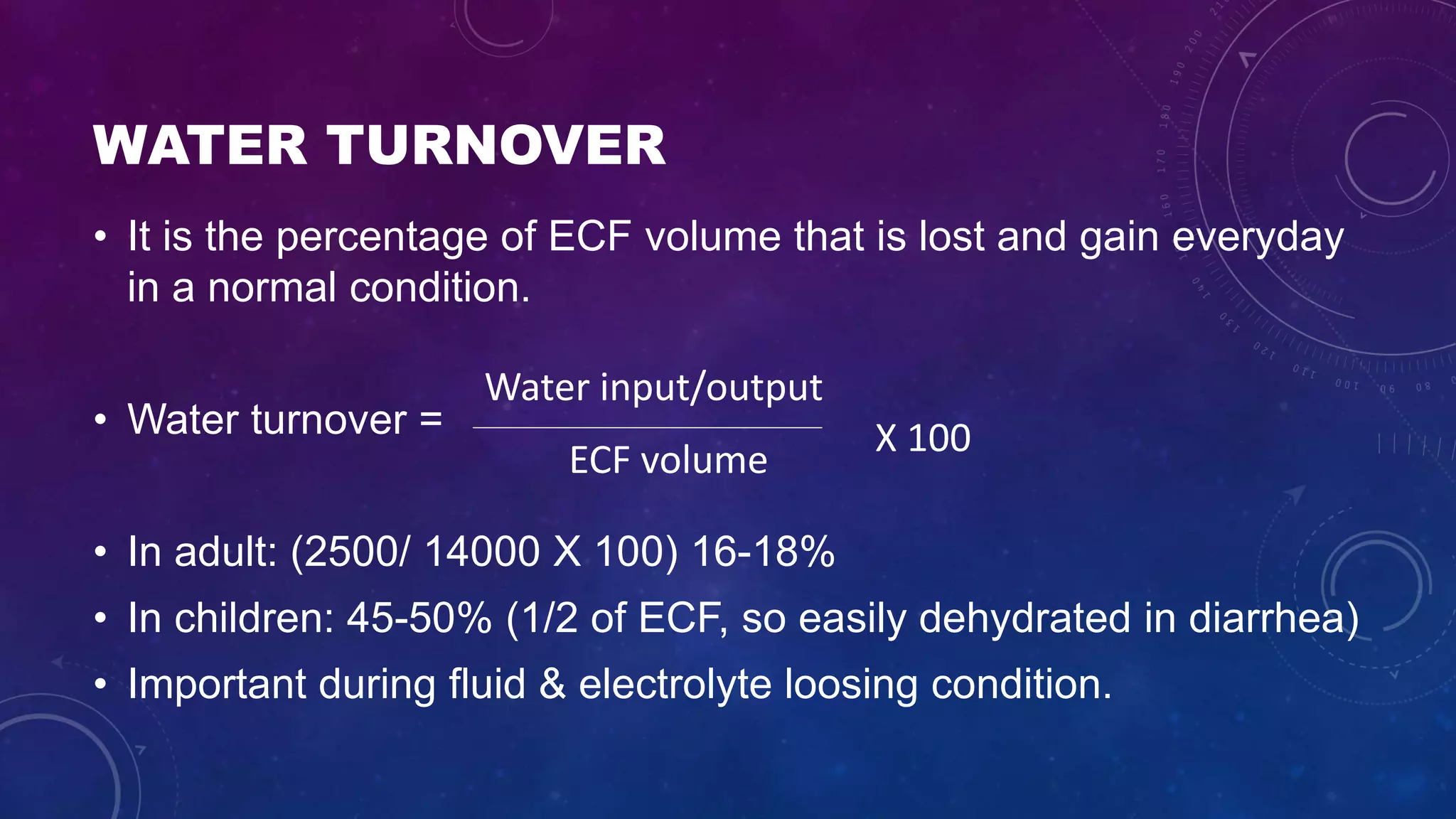
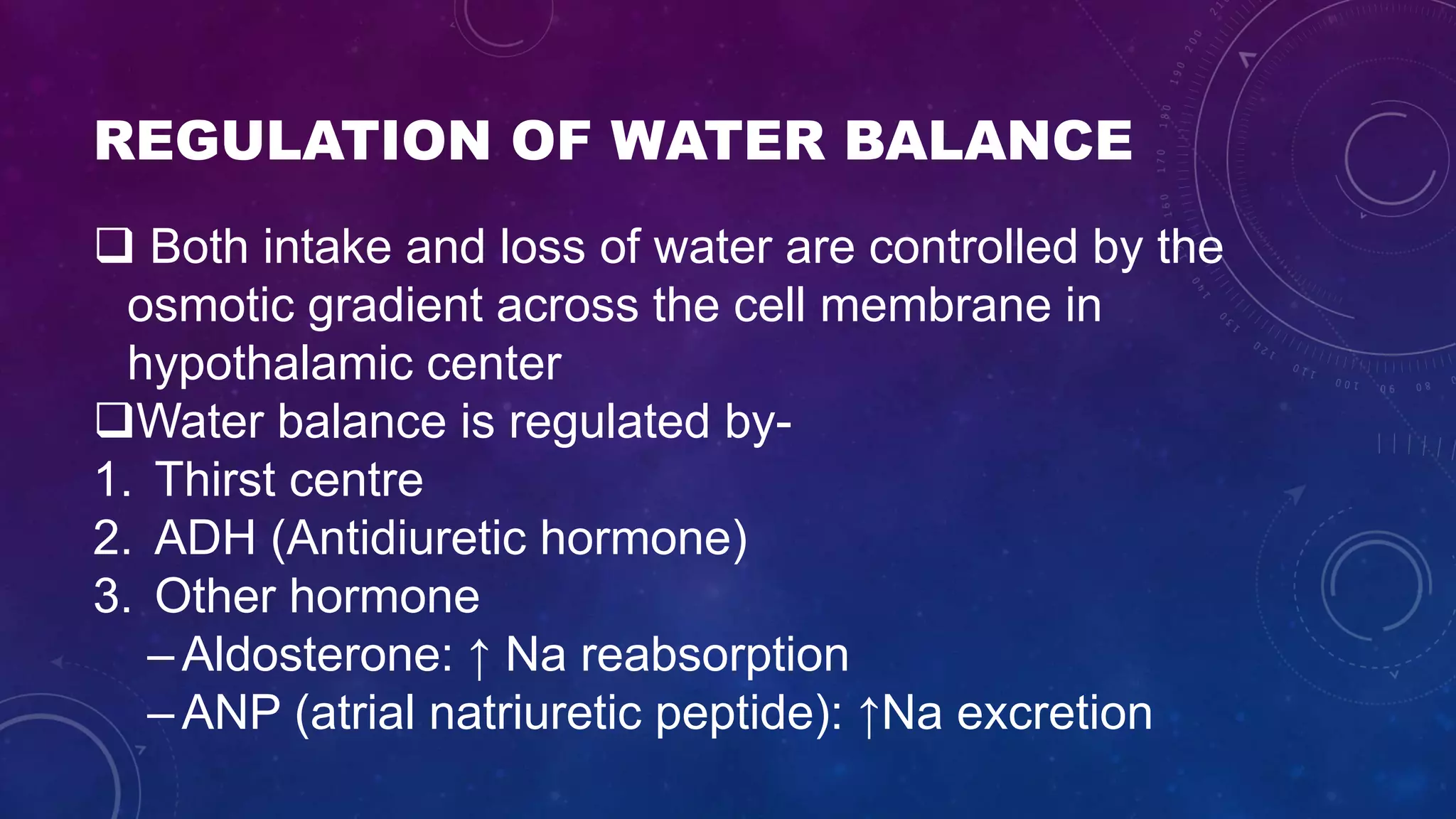
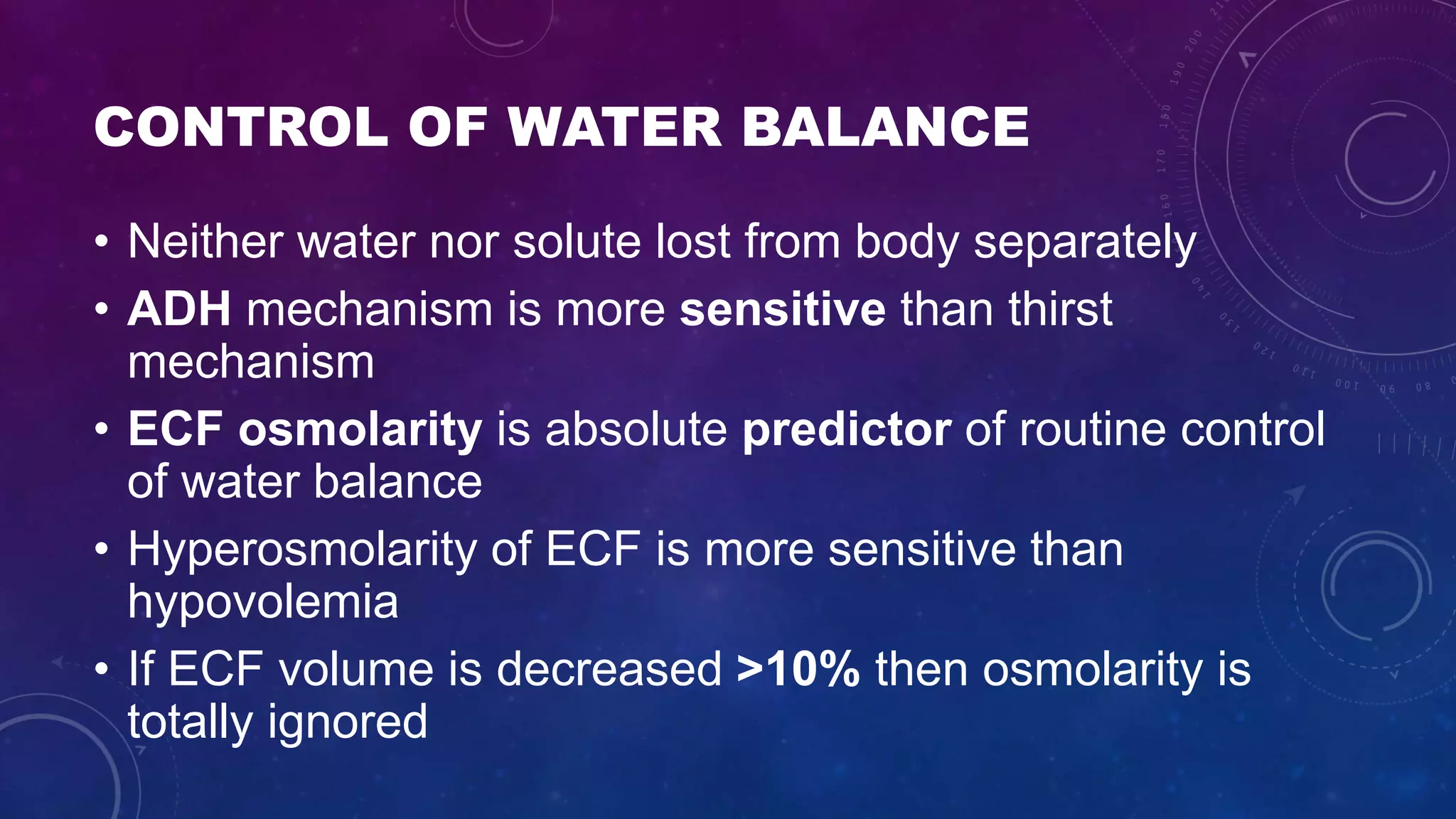
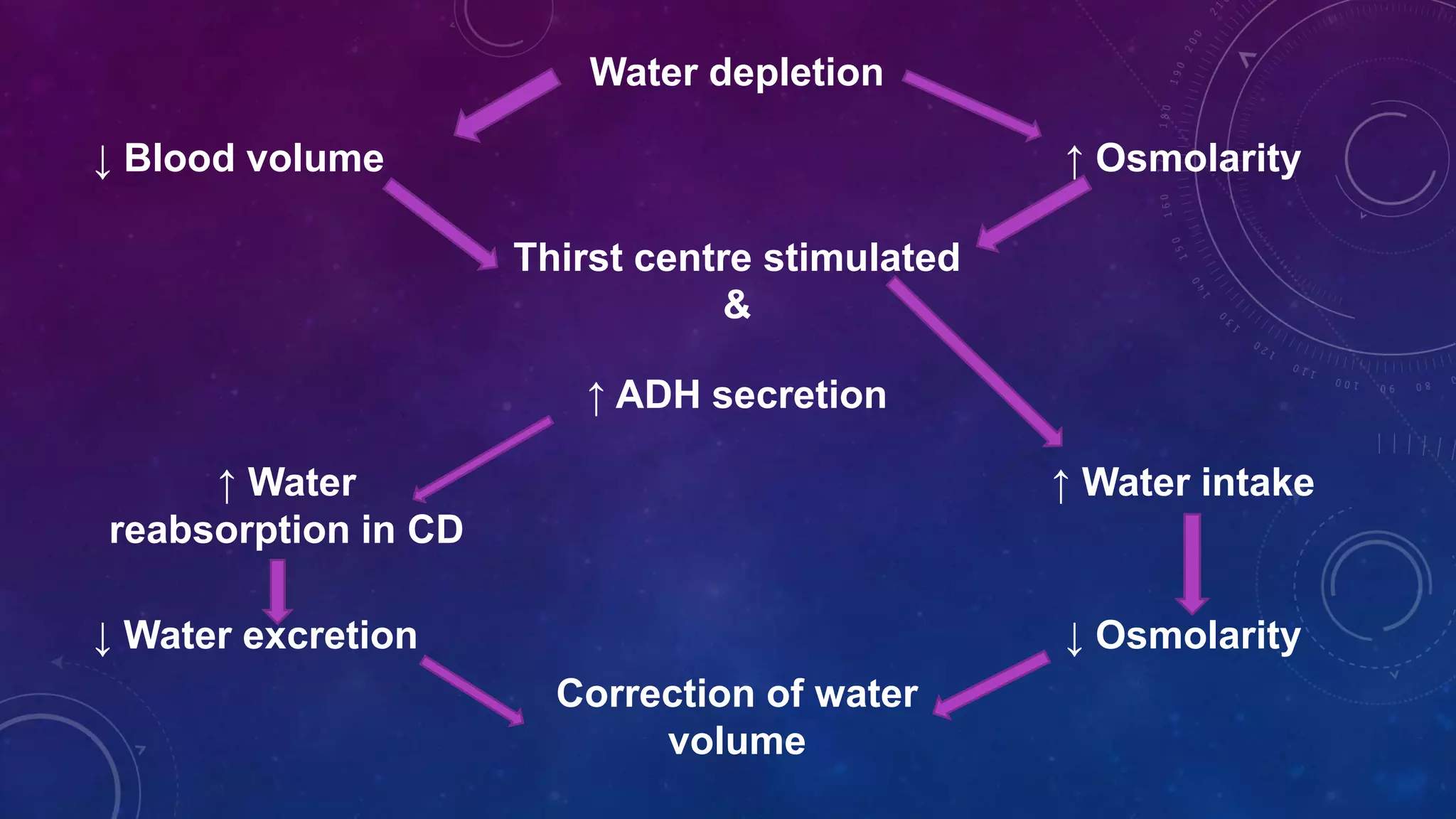
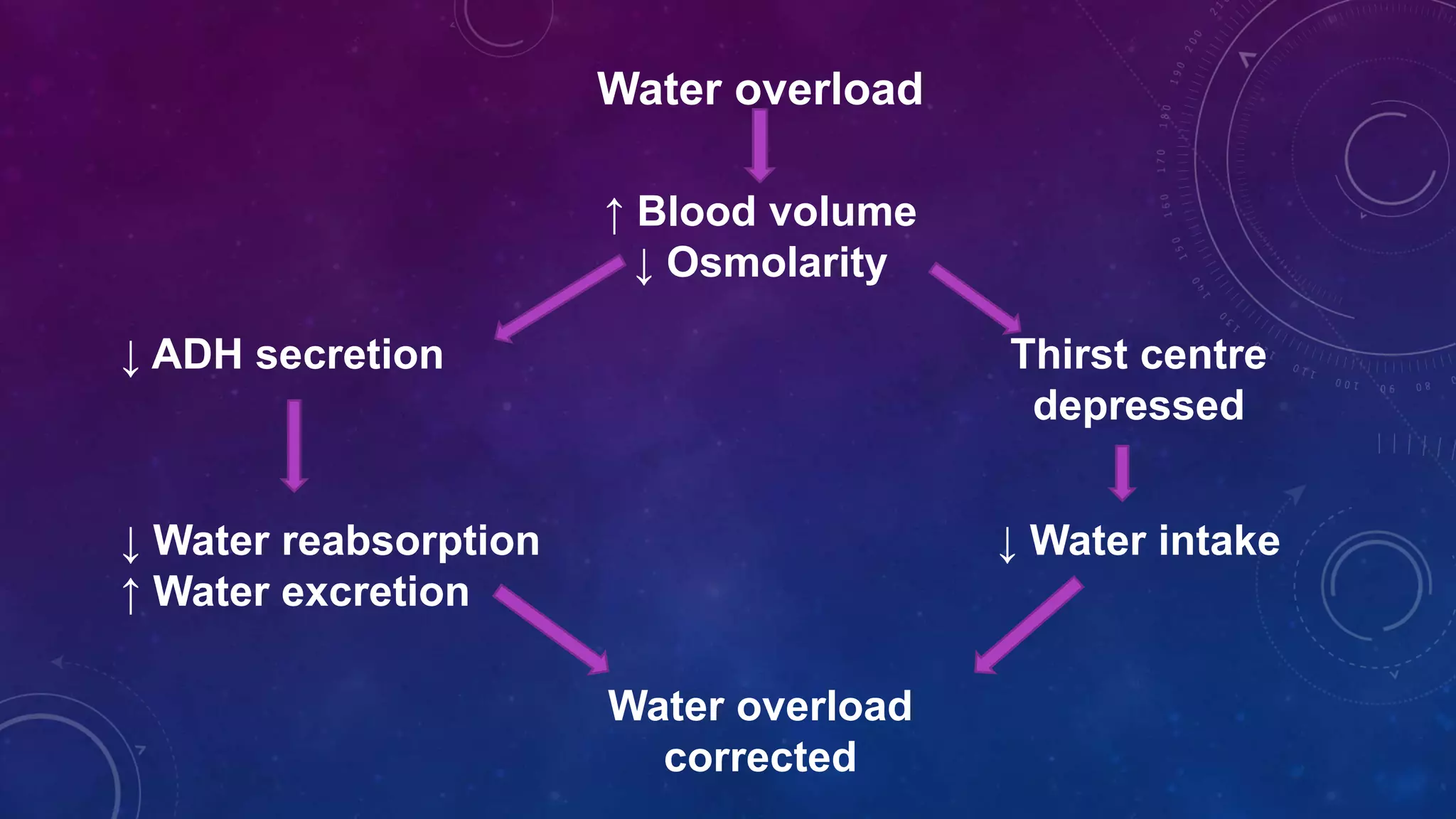
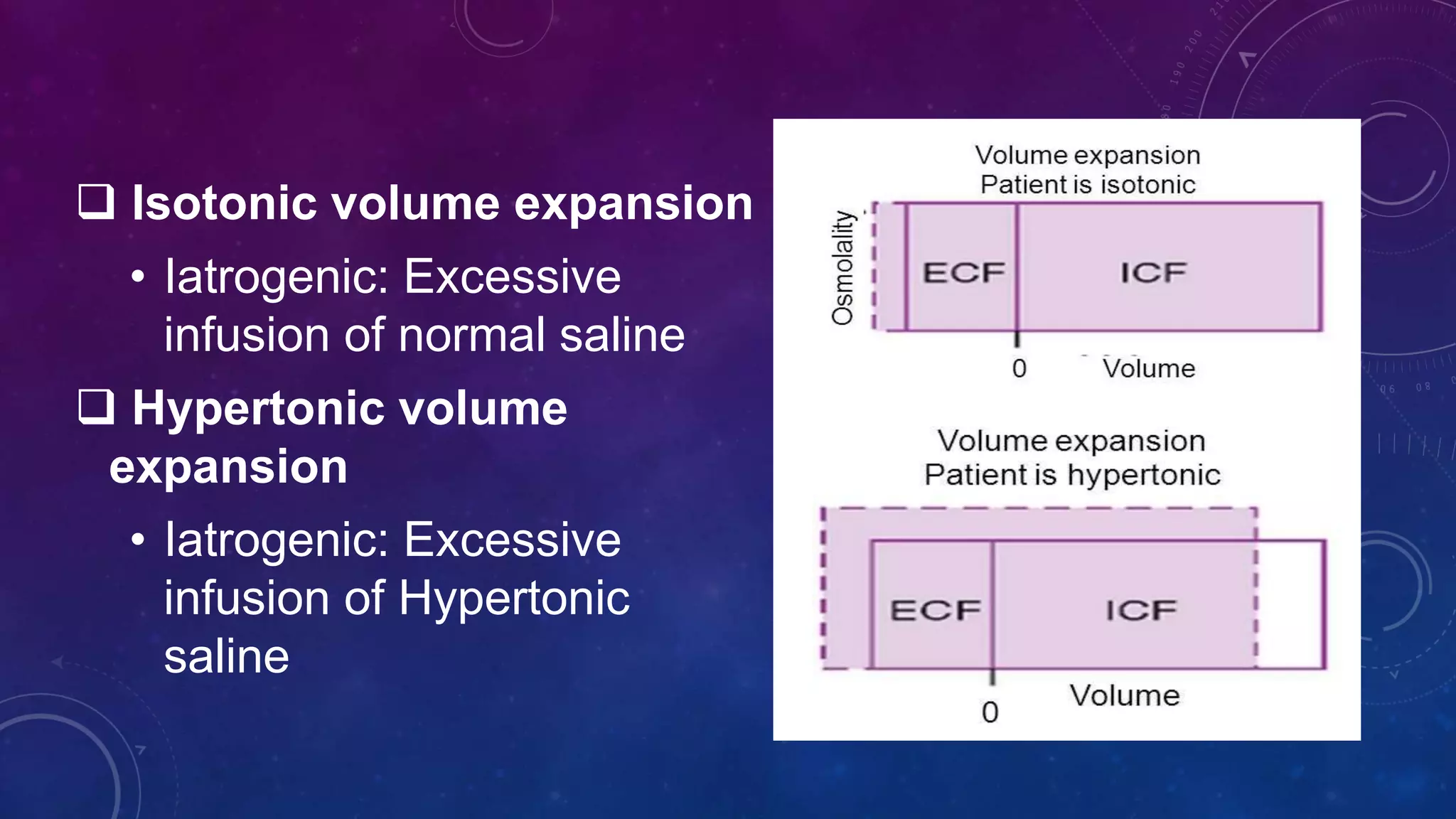
This document discusses body fluid distribution and regulation of water balance in the human body. It notes that total body water makes up 60% of body mass in males and 50% in females, with about two thirds being intracellular fluid and one third being extracellular fluid. Water balance is regulated by thirst, antidiuretic hormone, and other hormones in response to changes in extracellular fluid osmolality and volume. Disruptions to water balance can cause various volume disorders including isotonic, hypotonic, and hypertonic contractions or expansions.