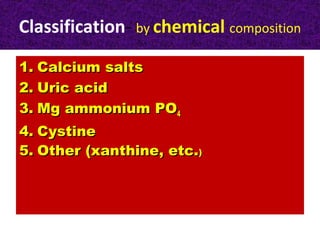
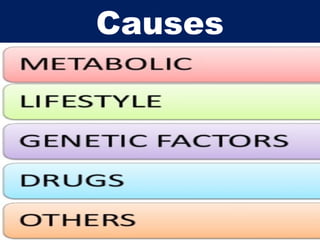
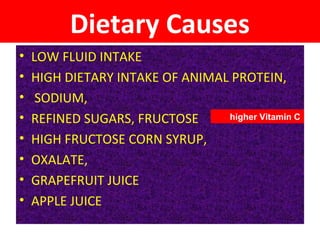
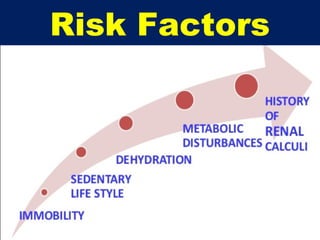
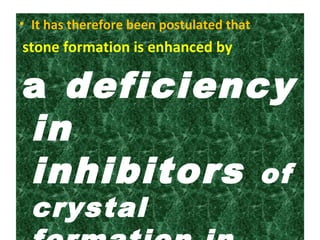
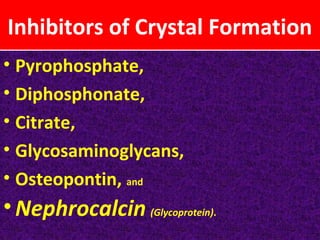
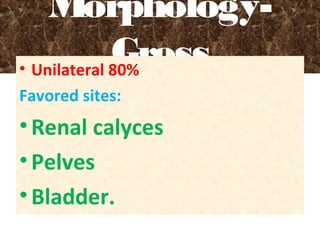
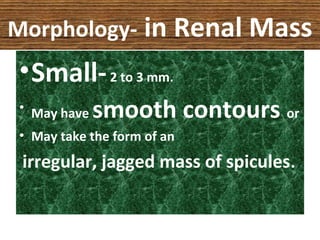
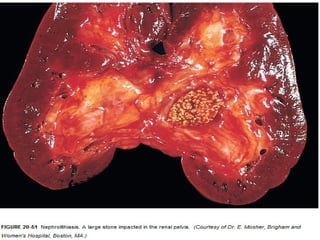
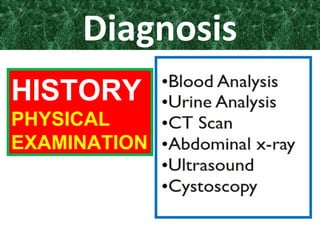
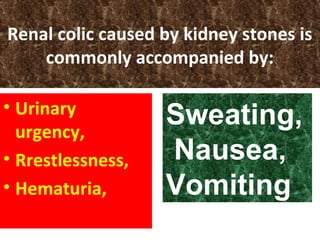
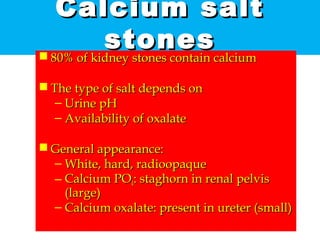
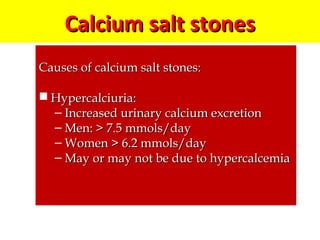
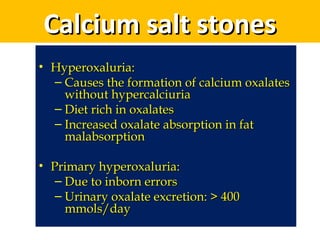
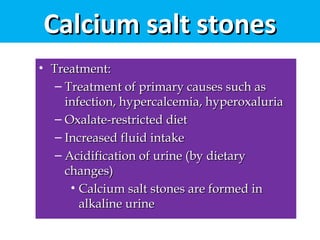
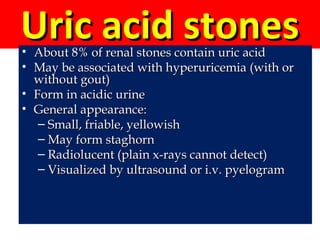
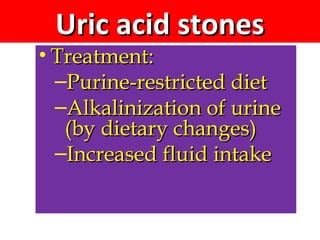
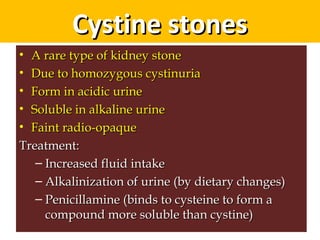
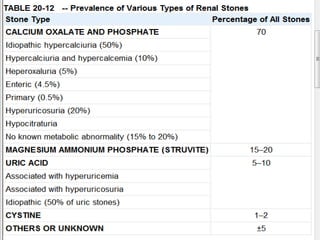
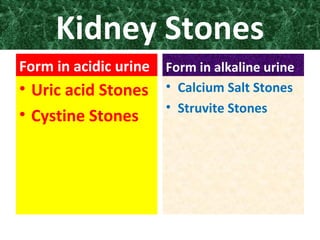
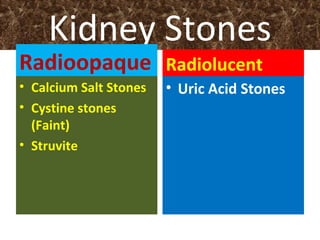
Kidney stones form when dietary minerals in urine become concentrated enough to crystallize. They are typically classified by location and chemical composition, with calcium salts and uric acid being most common. Risk factors include diet, medical conditions, and family history. Stones form through supersaturation when urine is too concentrated for minerals to remain in solution. Symptoms include flank pain, nausea, and blood in urine. Diagnosis involves history, physical exam, and imaging tests like ultrasound or CT. Treatment focuses on resolving underlying causes and preventing stone recurrence.