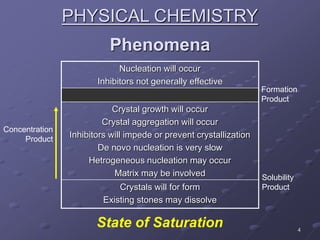
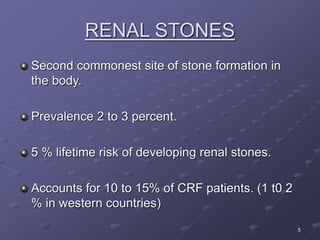
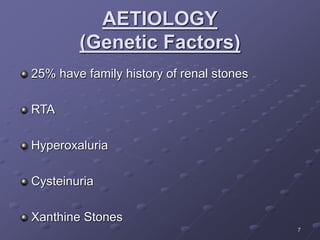
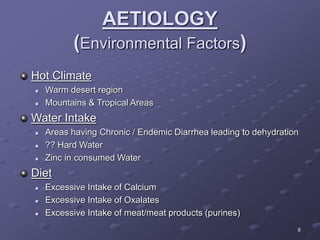
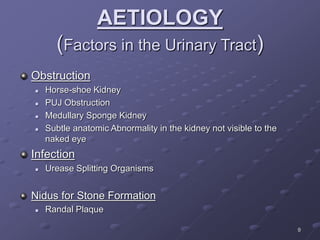
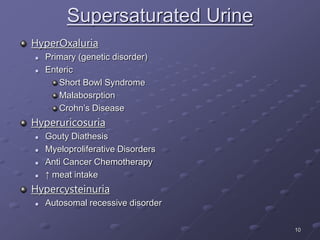
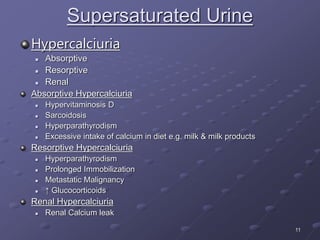
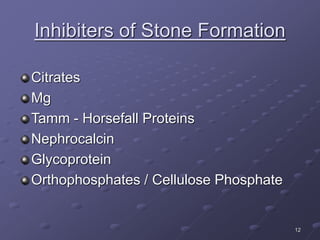
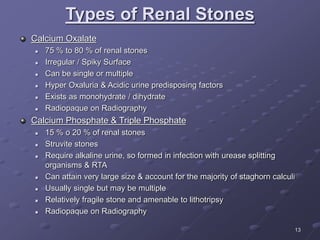
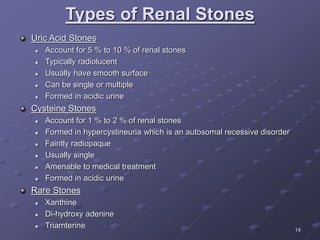
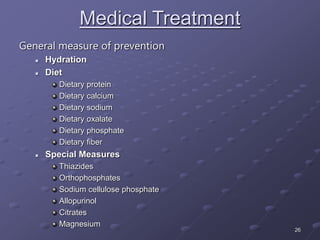
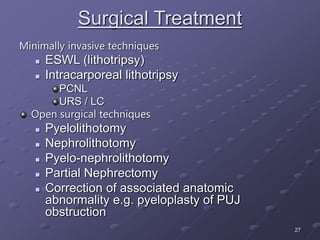
Urinary stones have been documented as far back as ancient Egypt. They form due to supersaturation of substances like calcium, oxalate, and uric acid in the urine. Risk factors include genetic factors, environmental exposures, and anatomical abnormalities of the urinary tract. Patients can be asymptomatic or experience flank pain, hematuria, and infection. Investigations include urine analysis, ultrasound, CT scans, and 24-hour urine collection. Treatment involves medical management of underlying causes, dietary modifications, and minimally invasive or open surgical procedures to remove stones.