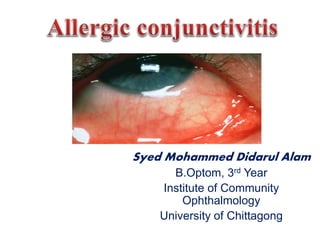
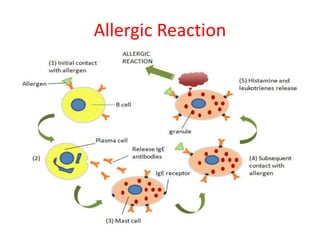
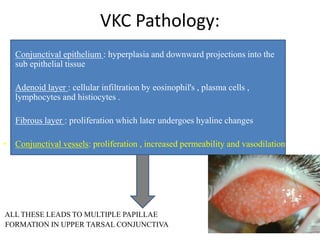
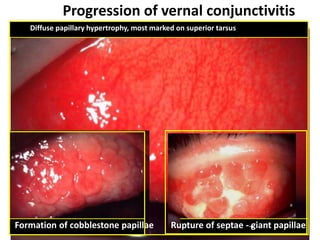
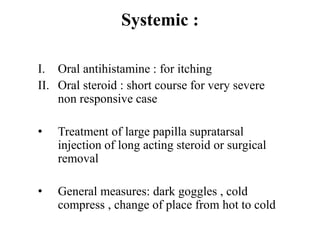
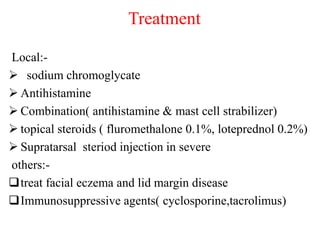
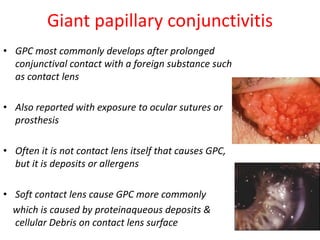
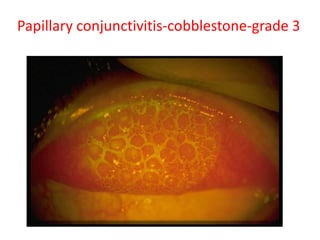
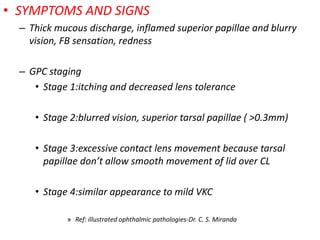
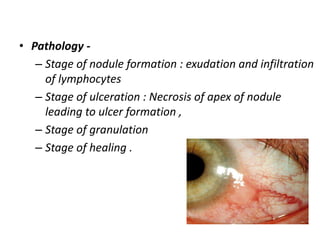
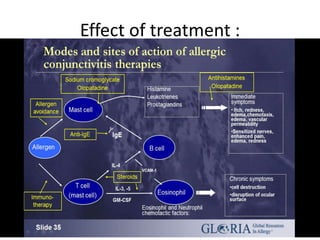
This document discusses different types of allergic conjunctivitis, including symptoms, signs, pathogenesis, and treatment. It covers simple allergic conjunctivitis like seasonal and perennial forms. It also discusses vernal keratoconjunctivitis, atopic keratoconjunctivitis, giant papillary conjunctivitis, phlyctenular keratoconjunctivitis, and contact dermatoconjunctivitis. For each type, the document provides details on clinical presentation, pathology, and recommended treatment approaches.