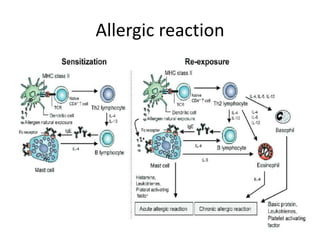
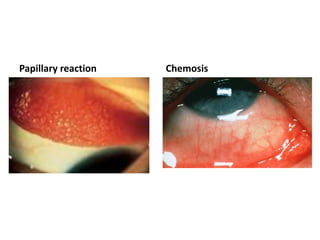
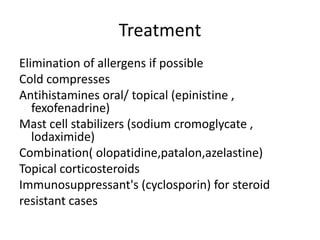
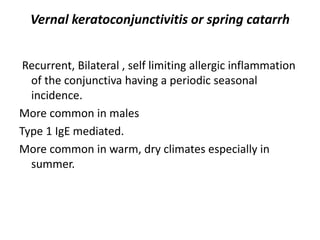
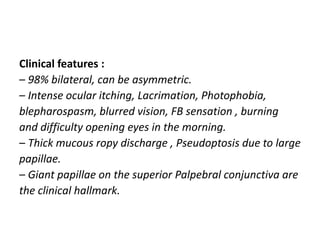
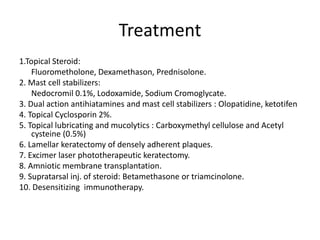
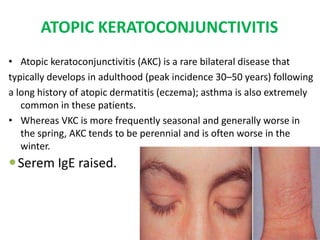
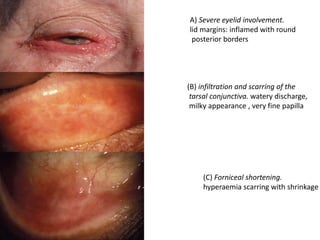
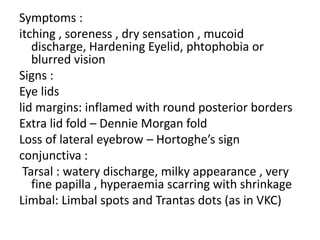
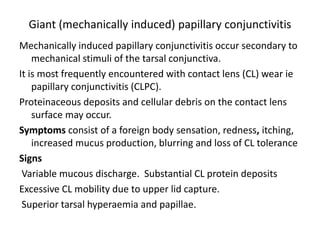
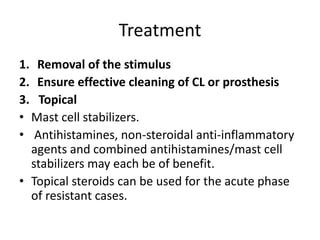
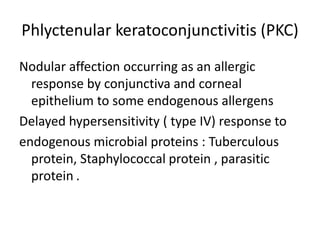
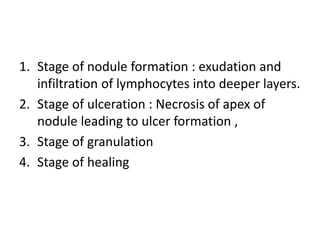
This document summarizes different types of allergic conjunctivitis. It describes a case of a 32-year-old woman presenting with itchy, red eyes and ropy discharge who was diagnosed with acute allergic conjunctivitis. It then discusses the different types of allergic conjunctivitis including simple allergic conjunctivitis, vernal keratoconjunctivitis, atopic keratoconjunctivitis, giant papillary conjunctivitis, and phlyctenular keratoconjunctivitis. For each type, it provides details on symptoms, signs, clinical features, and treatment options.
![Management
• She was diagnosed as Acute Allergic conjunctivitis
and managed on the following medications.
1. Gtt. Winolap [ Olopatidine 0.1%(w/v) – Dual action
antihistamines and mast cell stabilizers] BD 1 drop
B/E for 2 weeks.
2. Gtt. RefeshTear [Carboxymethyl cellulose
0.5%(w/v)] QID 1drop B/E for 1 month
3. Advice:
Avoid direct sunlight, dust and any other allergens.
Maintain ocular hygiene.
F/U after 2 weeks / SOS](https://image.slidesharecdn.com/allergicconjunctivitis-210609161207/85/Allergic-conjunctivitis-4-320.jpg)