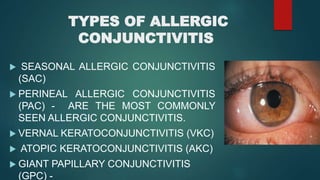
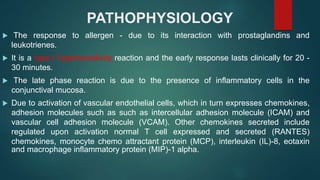
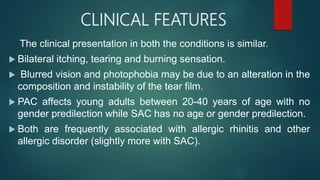
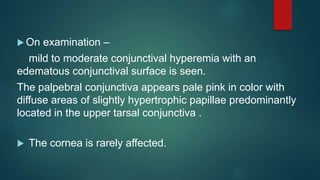
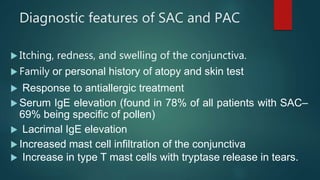
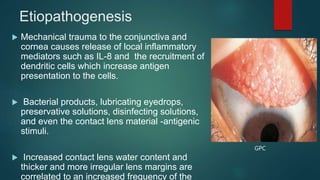
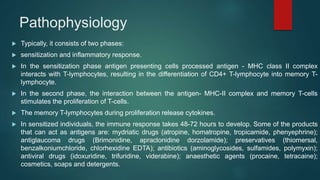
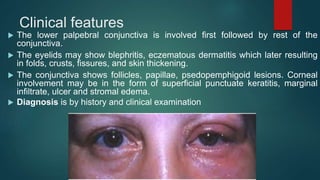
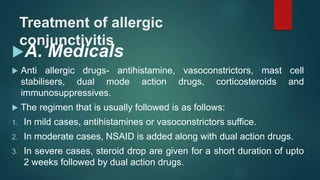
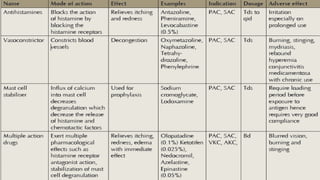
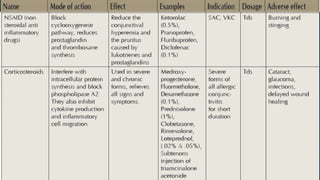
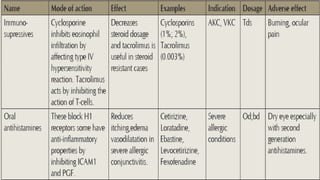
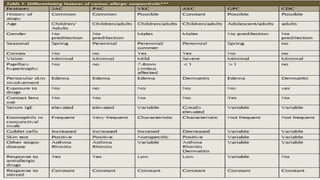
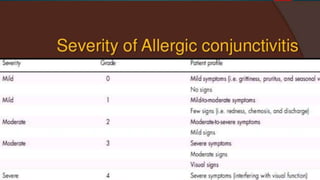
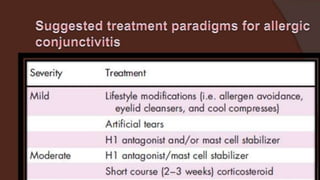
The document discusses ocular allergy and the various types of allergic conjunctivitis, describing their clinical manifestations, pathophysiology, diagnosis, and treatment approaches. The most common types are seasonal allergic conjunctivitis and perennial allergic conjunctivitis, both of which present with itching, tearing, and redness. The treatment involves anti-allergic medications, avoidance of allergens, and occasionally surgery for severe cases.