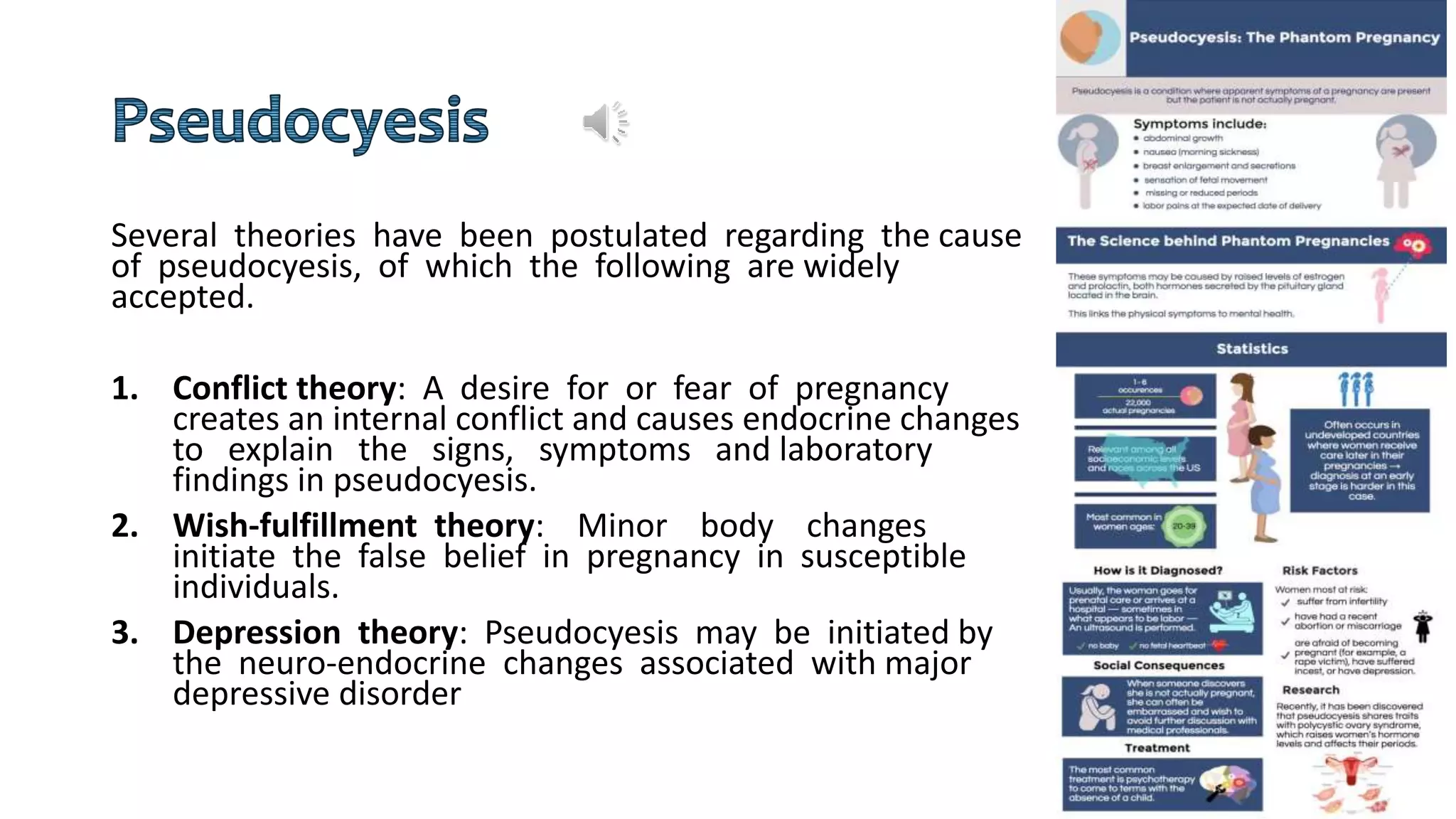
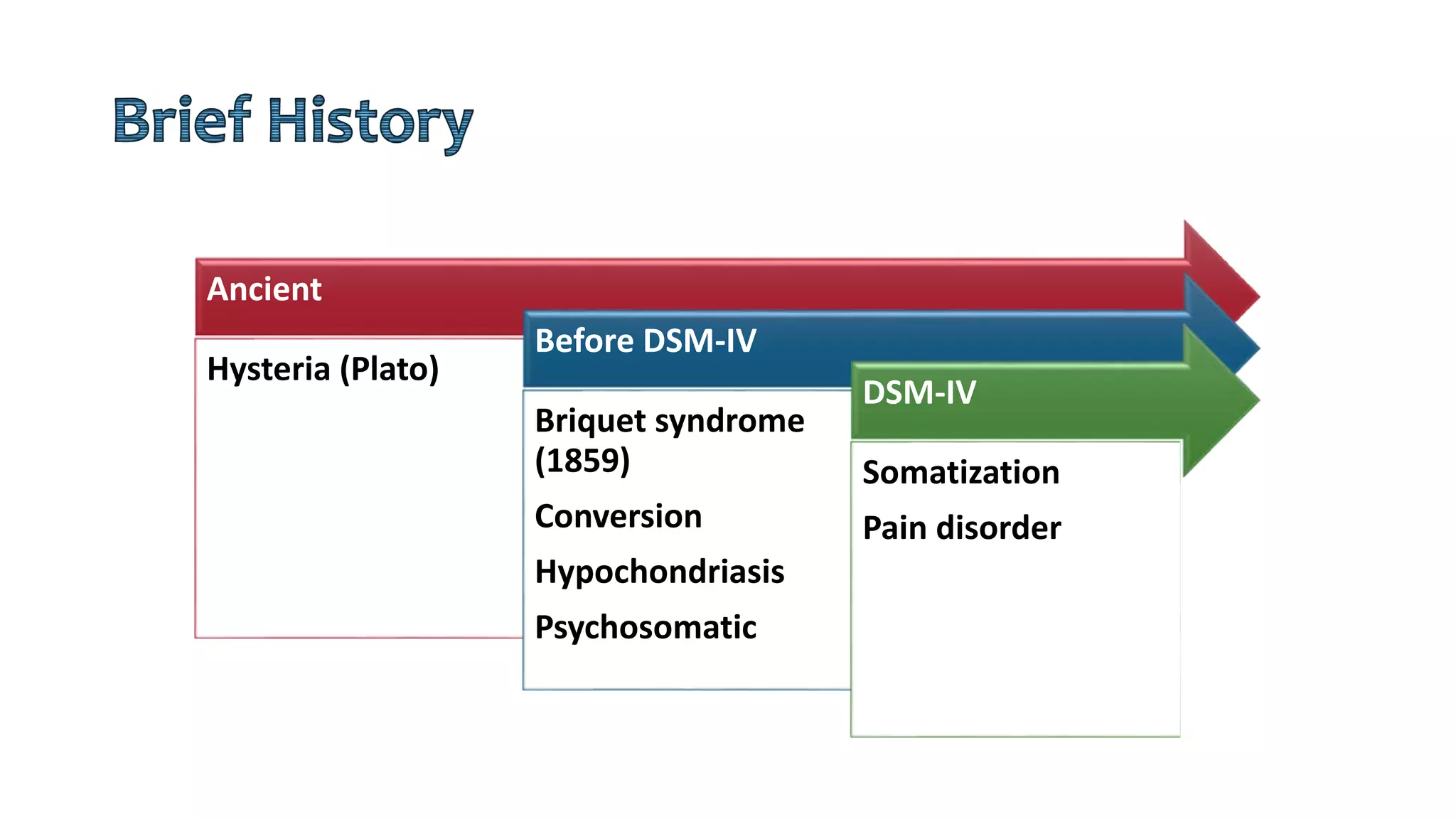
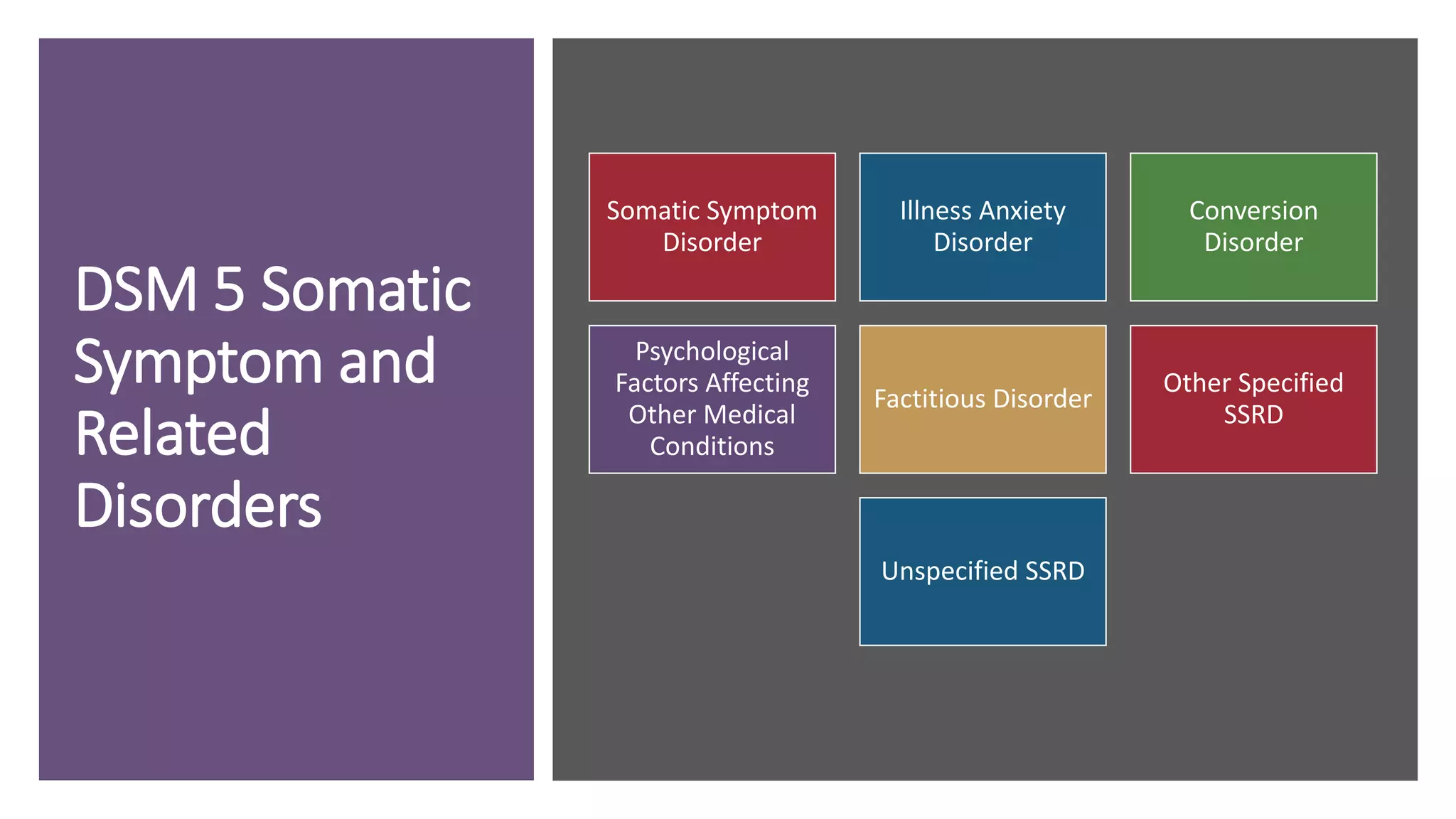
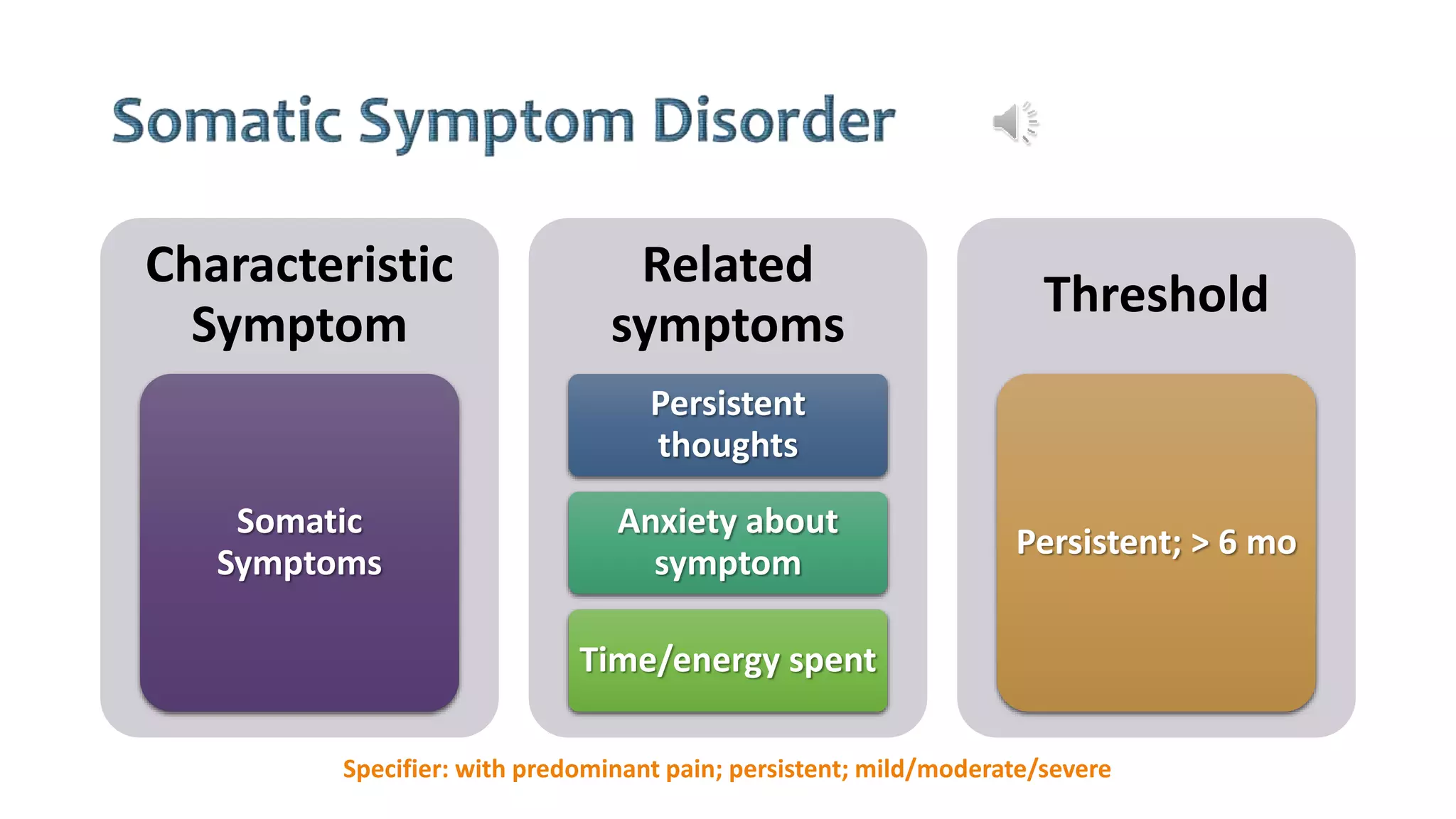
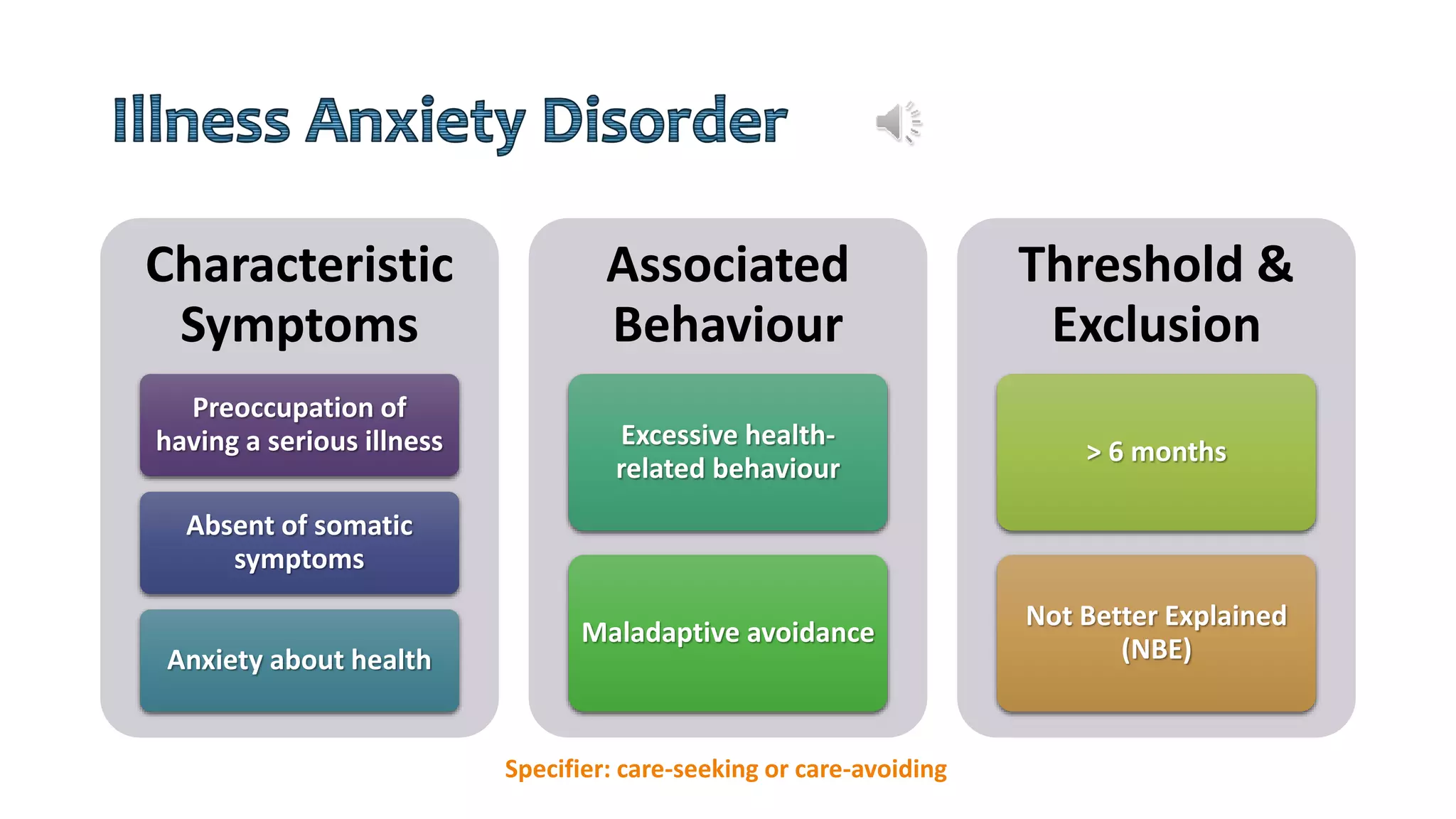
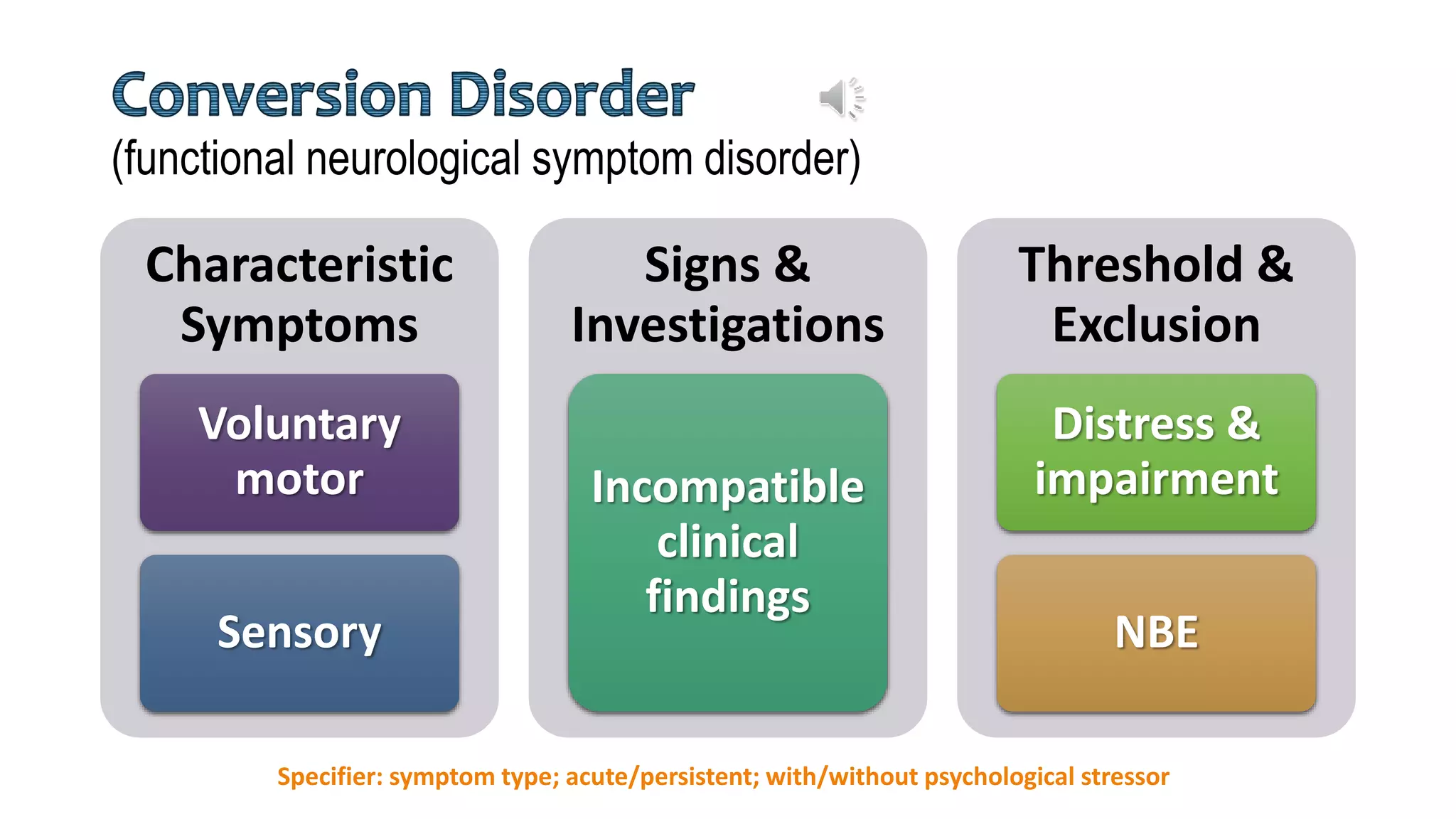
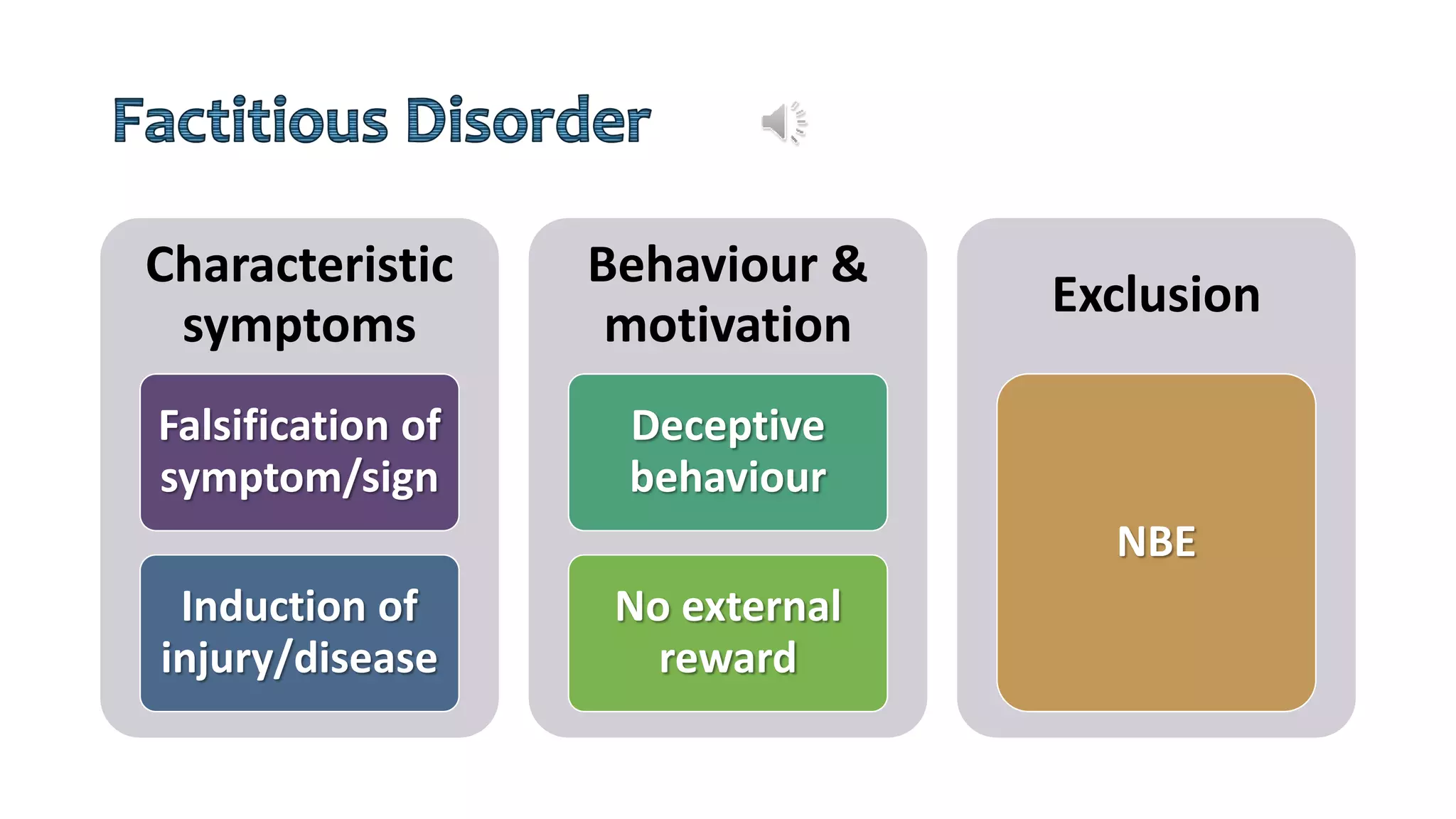
The document discusses the history and evolution of somatic symptom and related disorders. It describes how concepts like hysteria, hypochondriasis, and psychosomatic disorders developed before being categorized under somatic symptom disorder, illness anxiety disorder, conversion disorder, and other diagnoses in DSM-5. It provides details on the characteristic symptoms, thresholds, and specifiers for each DSM-5 disorder category. Theories on the causes of related conditions like pseudocyesis are also summarized.

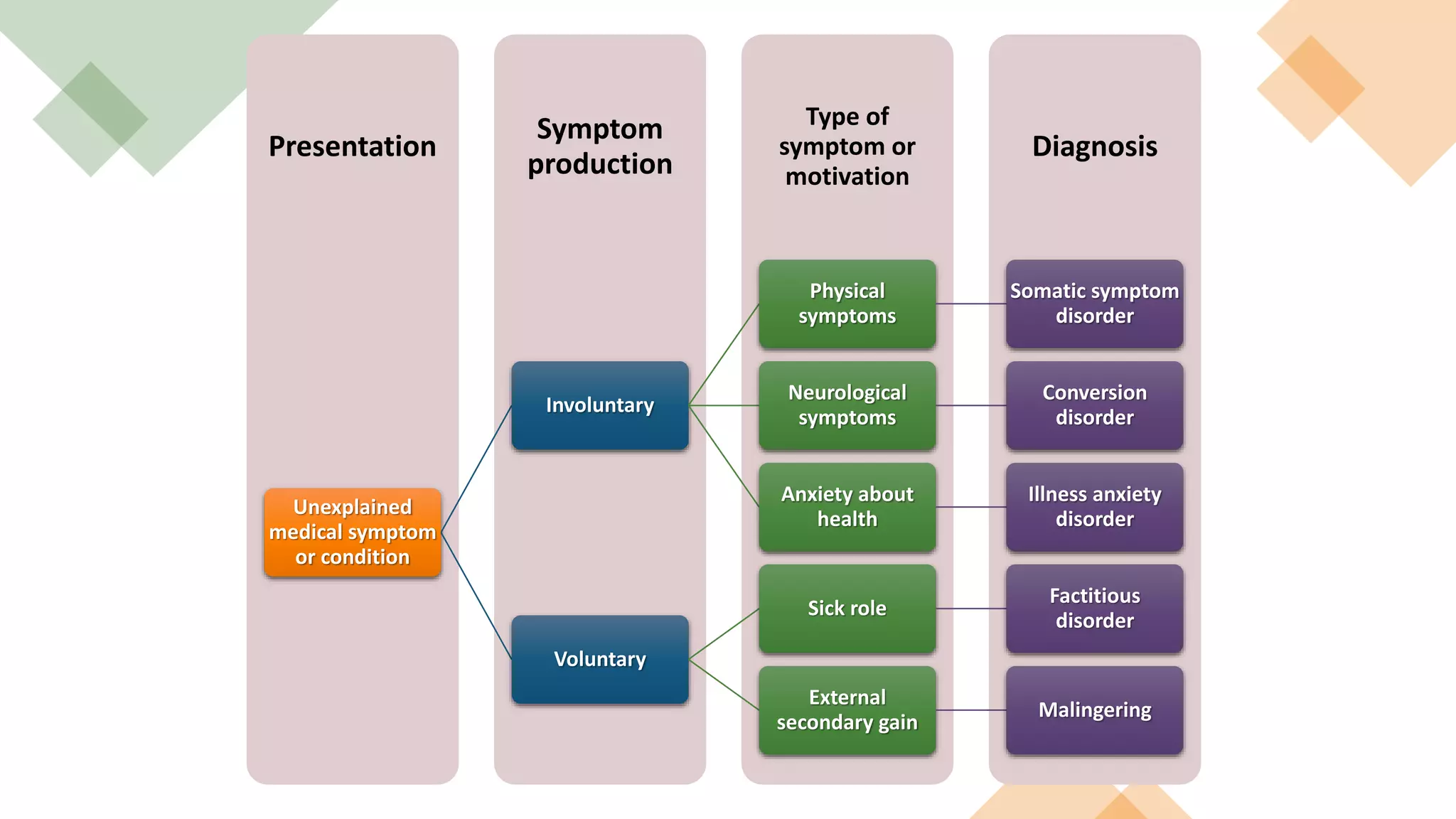
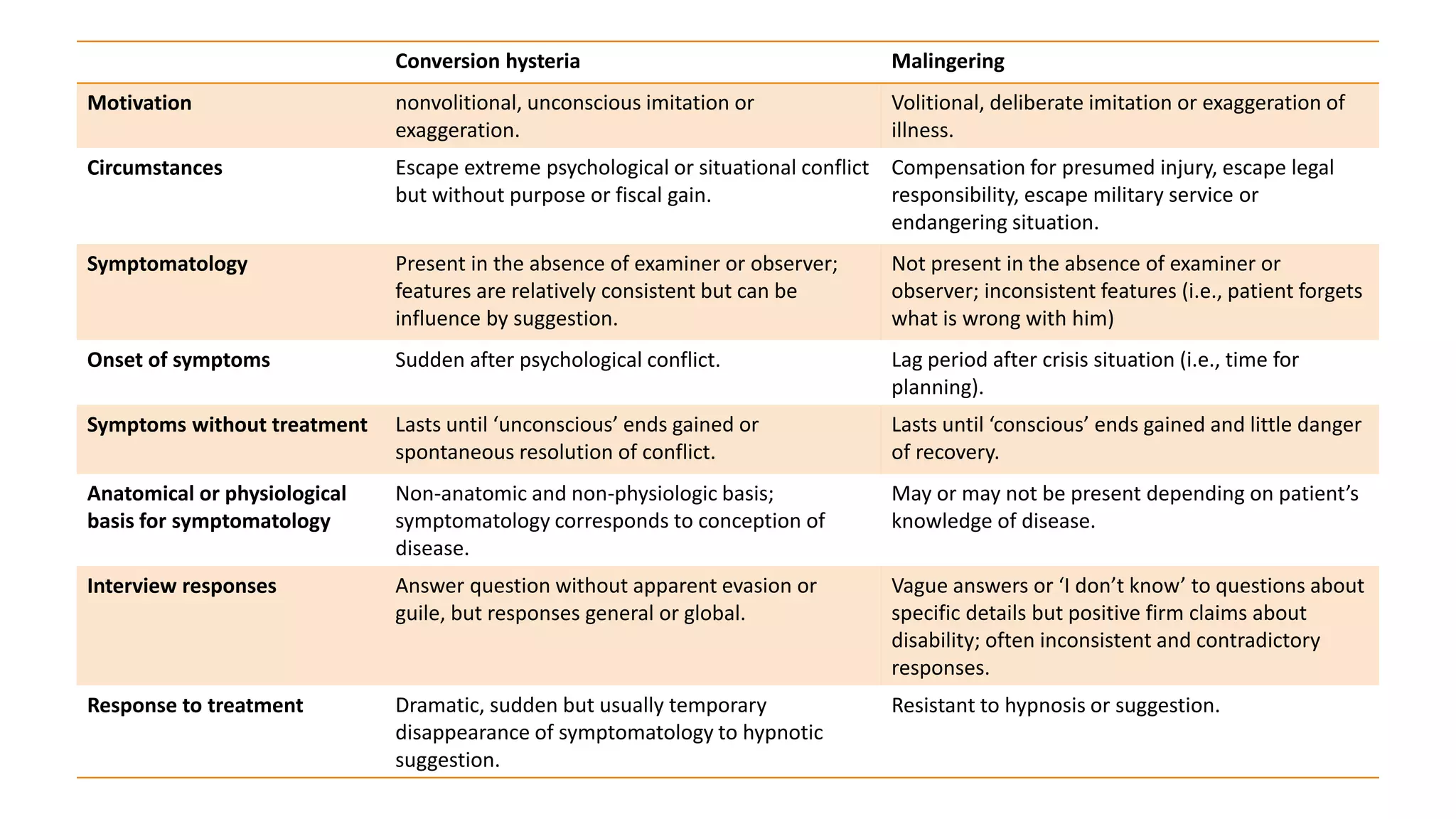
![Involuntary < --------------INTENTION------------- > Voluntary
Malingering
Factitious
Disorder
Compensation
Neurosis
Conversion Disorder
[DSM-5 Functional
Neurological Disorder]
Internal<----MOTIVATION---->External
Malingering is NOT a psychiatric disorder
Exaggeration <-----> Deception
Primarygain<----->Secondarygain](https://image.slidesharecdn.com/ssrdv1-200526002841/75/Somatic-Symptom-and-Related-Disorders-2020-12-2048.jpg)
![• The Greek word hypokhondria,
literally means “under the cartilage
(of the breastbone).”
• The upper abdomen, it turns out,
was thought to be the seat of
melancholy at a time when the
now-outdated medical theory of
the 4 humors (blood, phlegm,
yellow bile [choler], and black bile
[melancholy]) was accepted as a
basis for legitimate health practice.
• In the 17th century, hypochondriac
referred to people who suffered
from “depression and melancholy
without cause”.
https://doi.org/10.1176/ajp.141.12.1608](https://image.slidesharecdn.com/ssrdv1-200526002841/75/Somatic-Symptom-and-Related-Disorders-2020-19-2048.jpg)