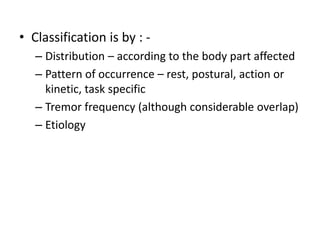
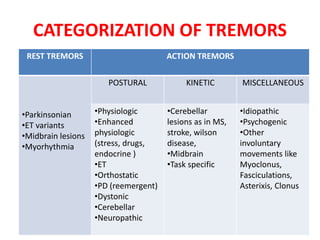
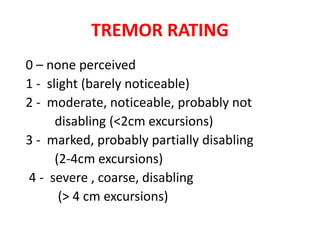
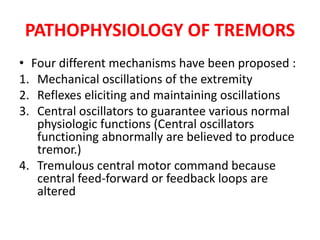
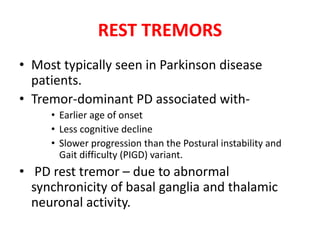
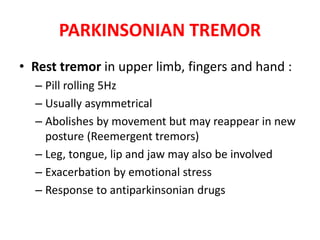
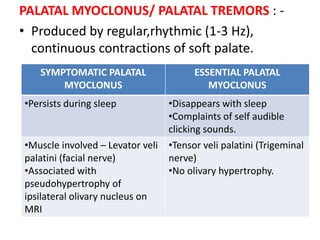
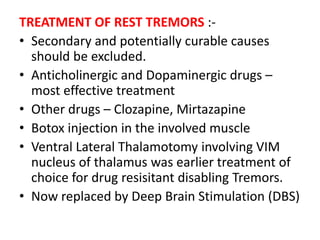
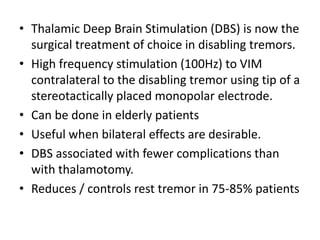
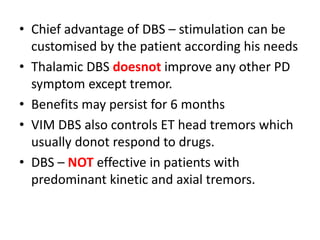
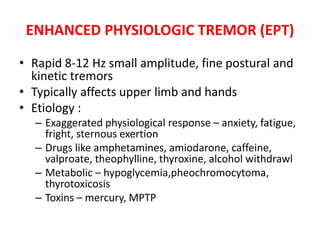
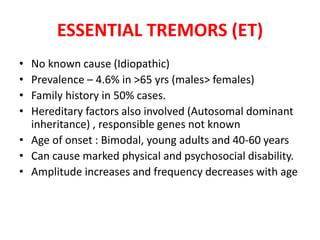
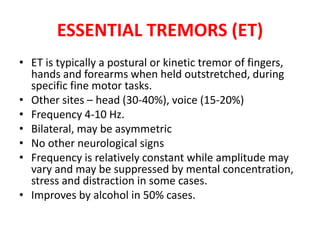
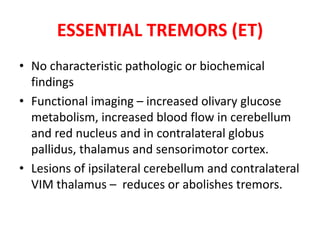
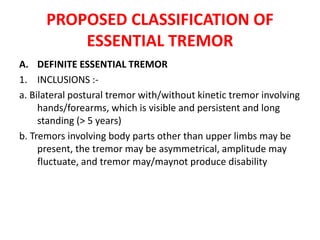
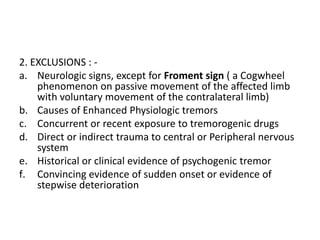
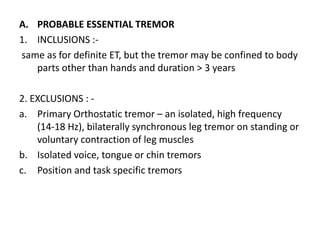
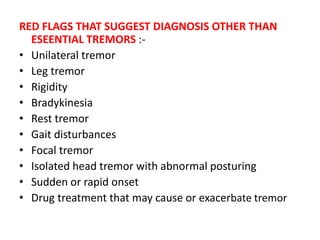
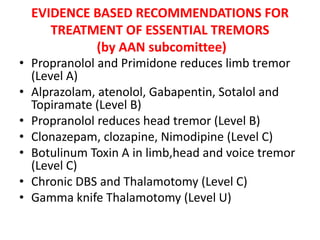
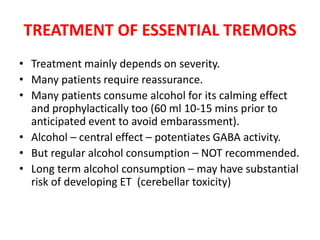
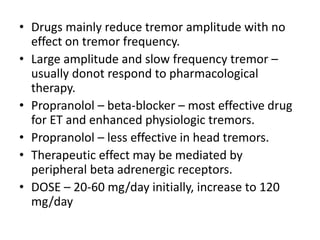
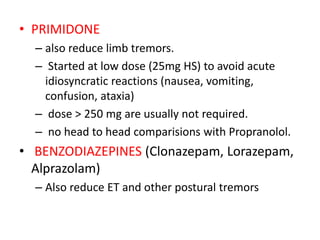
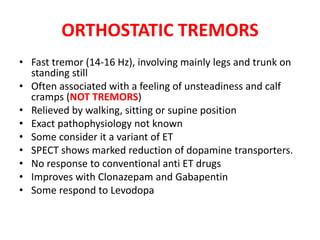
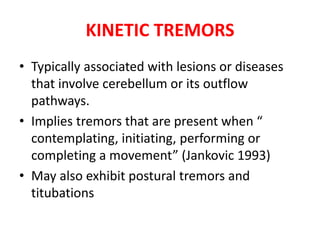
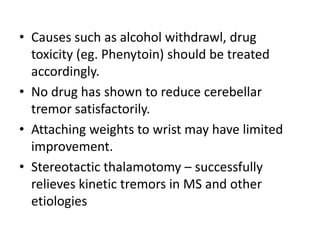
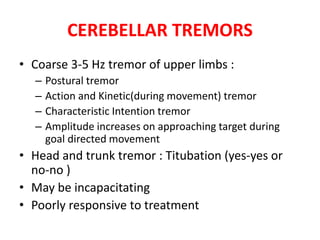
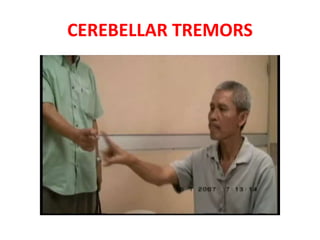
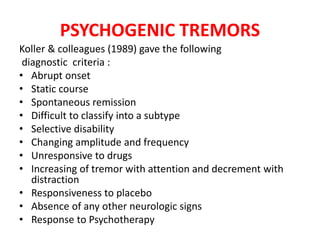
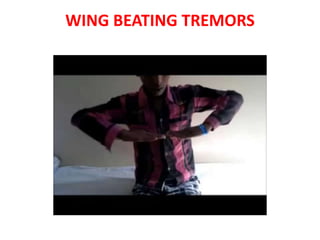
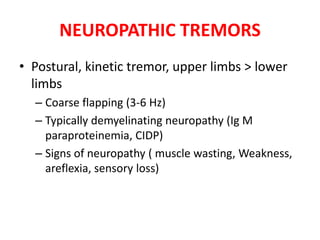
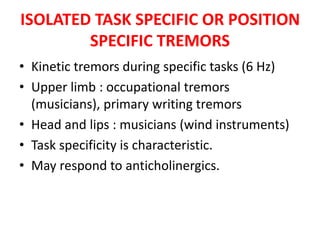
This document discusses different types of tremors, including their classification, causes, symptoms, and treatment. It covers rest tremors like Parkinsonian tremor and midbrain tremors. It also discusses postural tremors such as essential tremor and enhanced physiologic tremor. Treatment options covered include medications, botulinum toxin injections, deep brain stimulation, and thalamotomy.