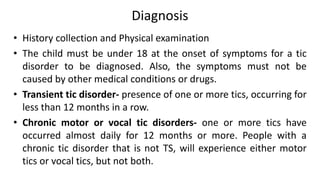
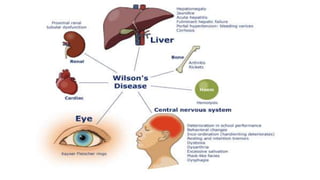
1. The document discusses various movement disorders including tics, dystonia, chorea, and Wilson's disease.
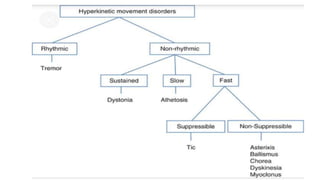
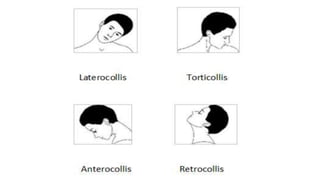
2. Tics are involuntary, repetitive movements or vocalizations that can be either simple or complex. Dystonia causes sustained muscle contractions resulting in twisting postures or movements.
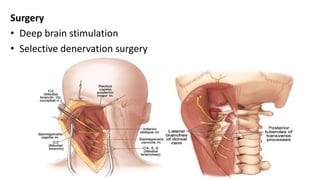
3. The causes, characteristics, classifications, and treatments of these various movement disorders are explained. Non-medication treatments include cognitive behavioral therapy, habit reversal therapy, and deep brain stimulation for severe cases.
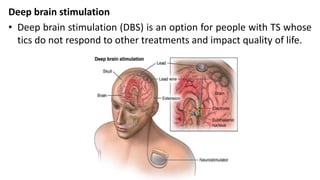




![RESEARCH ARTICLES
Effectiveness of a modified comprehensive behavioral intervention for tics for children and
adolescents with tourette's syndrome: A randomized controlled trial
A randomized controlled trial was conducted by Chia-Wen Chen, Huei-Shyong Wang, Hsiu-Ju
Chang, Chang-Wei Hsueh to evaluate the effectiveness of a modified four-session
Comprehensive Behavioural Intervention for Tics programme for decreasing tics in children
and adolescents with Tourette's syndrome. Participants aged 6-18 years with Tourette's
syndrome or chronic tic disorder were recruited. Participants in the control and intervention
groups (N = 23 each) received the routine care (daily pyridoxine [50 mg] and
psychoeducation). The intervention group received additional four behavioural intervention
sessions over a 3-month period that included psychoeducation, habit reversal training,
relaxation training, and education on tic relapse prevention. The outcome measures, Yale
Global Tic Severity Scale scores, were assessed at before and after the completion of
programme for both groups and again at 3 months follow-up for the intervention group.
Comparison of scores before and after intervention showed that the intervention significantly
decreased the severity of total motor tics and total tics as compared with control treatment.
The study concluded that modified four-session Comprehensive Behavioural Intervention
for Tics programme was more effective than routine care for decreasing tic severity in our
cohort of 6 to 18-year olds. This improvement was maintained 3 months after intervention.](https://image.slidesharecdn.com/movementdisorders-200913170751/85/Movement-disorders-86-320.jpg)
![REFERENCES
•Janice L. Hinkle, Kerry H. Cheever. Brunner and Suddarth’s Textbook of Medical Surgical
Nursing. 2015. New Delhi. Wolters Kluwer.14th Edition. Volume 2. Pg. no. 1812-1813.
•Lewis. Medical Surgical Nursing Assessment and Management of clinical problems.2015.
New Delhi. Elsevier. 2nd Edition. Volume II. Pg. no.1498.
•Wikipedia. Tic. Available from
https://en.wikipedia.org/wiki/Tic#:~:text=A%20tic%20is%20a%20sudden,eye%20blinking
%20and%20throat%20clearing. [cited 1 sep 2020]
•MAYO CLINIC. Wilson’s disease. Available from https://www.mayoclinic.org/diseases-
conditions/wilsons-disease/diagnosis-treatment/drc-
20353256#:~:text=Your%20doctor%20inserts%20a%20thin,mutations%20that%20cause%
20Wilson's%20disease. [cited 2 sep 2020]
•PubMed. Effectiveness of a modified comprehensive behavioral intervention for tics for
children and adolescents with tourette's syndrome: A randomized controlled trial.
Available from https://pubmed.ncbi.nlm.nih.gov/31782167/ [cited 8 sep 2020]
•PubMed. Tremor in Dystonia: A Cross-sectional Study from India. Available from
https://pubmed.ncbi.nlm.nih.gov/30868097/ Mov Disord Clin Pract. 2017 Oct 3;4(6):858-
863. doi: 10.1002/mdc3.12546. [cited 8 sep 2020]](https://image.slidesharecdn.com/movementdisorders-200913170751/85/Movement-disorders-89-320.jpg)

